Canadian doctors co-signing prescriptions for U.S. patients
Canadian doctors are co-signing prescriptions for American patients they haven't seen — a practice critics consider unethical and one that violates every province's standards of care, CBC News has learned.
Prescriptions written by U.S. physicians require a co-signature from a Canadian doctor before a Canadian pharmacist can legally fill them.
Canada's internet pharmacies wouldn't be able to operate legally without the practice of co-signing,
but from the beginning it's been the source of controversy and debate.
"Each member keeps their own Canadian physician for doing the Canadian co-signing," said Tim Smith, general manager of the Canadian International Pharmacy Association (CIPA), which represents 64 websites operated by the 11 members of the industry group.
"The process is: We obtain the prescription from the physician who has examined the patient. That is sent to us at the time of the initial contact. We also obtain medical and demographic information to make sure there is no drug interaction. We understand the medical information about the patient.
"That information is shared with the Canadian physician and at that point, the Canadian physician will review it and if there are any concerns about what's prescribed or what other medications the patient might be on, then we go back to the patient. We'll also go back to the physician to have a discussion about that until the matter is cleared up," he said.
Smith wouldn't say how many Canadian doctors are co-signing American prescriptions for CIPA members or which provinces license them, although he did confirm none are licensed in Manitoba.
However, it's against the standards of care for doctors in every province to prescribe drugs without a direct physician-patient relationship.
In Manitoba, the College of Physicians and Surgeons has a specific formal statement that member physicians must comply with:
"Prescribing of medications by physicians based solely on information received without direct patient contact fails to meet an acceptable standard of care and is outside the bounds of professional conduct. There is no direct patient contact when the physician relies upon a mailed, faxed or an electronic medical questionnaire or telephone advice to the physician."
"In order to meet an acceptable standard of practice, the physician must demonstrate that there has been:
- A documented patient evaluation by the Manitoba physician signing the prescription, including history and physical examination, adequate to establish the diagnosis for which the drug is being prescribed and identify underlying conditions and contra-indications.
- Sufficient direct dialogue between the Manitoba physician and patient regarding treatment options and the risks and benefits of treatment.
- A review of the course and efficacy of treatment to assess therapeutic outcome.
- Maintenance of a contemporaneous medical record that is easily available to the Manitoba physician, the patient, and the patient's other health care professionals."
"If they're Manitoba doctors who are doing that, they are contravening our statement and should be reviewed," registrar Anna Ziomek said, adding the college needs a written complaint in order to investigate. That would include any information gathered in investigations by other health-care regulatory bodies.
There are some exceptions. For example, a physician who is part of a call group and responsible for looking after other doctors' patients during off-hours can authorize a refill of a prescription written by another member of the group. The doctor must then notify the primary physician.
Another exception is in remote communities where doctors might only be reached by phone.
At least 27 physicians were disciplined in eight provinces between 2003 and 2012 for co-signing foreign prescriptions, including 10 from Manitoba. Punishments have included censure, and orders to pay costs. In one case the doctor in question was fined $25,000.
"I don't think it's ethical for a Canadian doctor to prescribe medicine to a patient he or she has never seen," Amir Attaran a professor of law and medicine at the University of Ottawa, told CBC News.
"I think frankly those doctors should have their licences pulled, because how can you prescribe medicine for a patient who you know nothing about?" said Attaran, who has studied Canada's internet pharmacy industry for years.
"You don't know what other drugs that patient is taking. You may be prescribing a medicine that interacts with those drugs and that interaction can even be deadly."
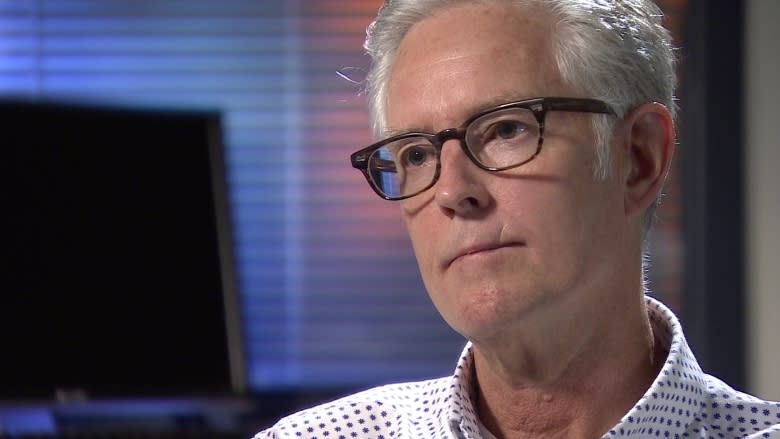
David MacKay, the former executive director of CIPA, disagrees. He believes having two doctors review a prescription adds a second level of safety.
"The co-signing process can be and is 'life-saving,'" MacKay said, adding this applies only when the drugs are Health Canada approved and come from Canadian pharmacies.
Rigorous oversight needed
However, without rigorous and independent global regulatory oversight, the supply chain of international pharmacies that provide some of the industry's prescription drugs could be exposed to a greater risk of counterfeit medication, MacKay added.
"If I were a co-signing physician I would be concerned about where the pharmacy is sourcing their medications, how they are being procured and what the supply chain looks like. If it involves a long and winding road through various countries to get to the U.S. patient then I wouldn't be putting my name on it," he said.
"That's placing a lot of trust in a process that is more prone to supply chain penetration despite all good intentions. I wouldn't do it."
In a follow-up interview, CIPA's Tim Smith said physicians working with his member pharmacies are required to follow the rules of the provinces in which they're licensed.
"Not turning a blind eye at all. What I'm suggesting is they are, we are, operating in compliance," he said.
However, Smith said, he would follow up on the co-signing question.
"I would certainly want to follow up on situations that were out of compliance. We're very proud of our record of compliance and we're very proud of the service we provide to many people, uninsured Americans. So certainly we would do what we needed to do," he said.