Doctor hits the road to deliver palliative care to Toronto's homeless
Dr. Naheed Dosani is a palliative care doctor in Toronto but his patients are not in hospitals and clinics, they're in homeless shelters, drop-in centres and sometimes even on the streets.
His patients are the city's homeless, an ebbing and flowing population that numbers approximately 5,000.
"When you're socially isolated on the streets, who's advocating for you?" he asks rhetorically.
Well, he is.
Thanks to a program called Palliative Education and Care for the Homeless (PEACH), funded by Inner City Health Associates via the Ontario Ministry of Health and Long-Term Care. Right now, PEACH is Dosani, but ICHA hopes to be able to fund a second mobile unit soon.
He gets into his Honda Civic every day and goes to see his patients wherever they may be.
"It's borderless," he told CBC News on a recent ride-along, and said people call his car "the PEACH-mobile."
Dosani dispenses much-needed health care to a vulnerable and marginalized population — many of them at the end of their lives.
'It's a tragedy'
"Our experience shows us that the majority of this population dies in social isolation," he says. "They die with very few people around them, very few supports, and it's a tragedy."
Dosani winds his way through city traffic, and arrives at Kensington Hospice, a 10-bed palliative care home located in a quiet Toronto neighbourhood.
He's there to check in on Andy Thomas, who's been in and out of shelters for 15 years. Dosani enters the dimly lit room with Leslie Randl, a palliative care co-ordinator with the Toronto Central Community Care Access Centre.
"Andy, how are you feeling today?" Dosani asks.
Andy is 43 and near death. He has metastatic stage 4 bladder cancer. Dosani and his team were able to secure this hospice bed, where in all likelihood Andy will spend the last few days of his life.
"The obstacles to a quality end of life for this population start to mount up, start to add up to a point where it's relatively impossible," says Dosani. "Andy is totally one of the lucky ones who is able to ... [be] in a hospice setting."
Andy is on a cocktail of medication including methadone and hydromorphone to manage the pain, and something for delirium.
On the day we visited, he was lying in his bed, weakened by his disease, but he mustered up enough strength to say that being in the hospice "releases as much of the stress as possible." If he wasn't here, where would he be? "Oh, the streets," he whispers. "Easily on the streets. There's nowhere else."
Andy has been estranged from his family for a decade. The only thing he really cares about, his two cats, are now staying with a friend.
On the way out, Dosani leans close to Andy's face. "You're really strong, Andy. Hang in there, OK? Get some rest."
The palliative care team is "most likely" his only family, says Dosani. "That's why today's visit was so important. It wasn't just a check-in. It was people he's known and built bridges with, bonds with, relationships with over time."
'I put myself in this position'
We're back in the PEACH-mobile, heading for a shelter in Toronto's east end.
Dosani's second patient of the day, 63-year old Miki Senisin, is waiting for him in the lobby. An unlit cigarette hangs from his mouth. He's an imposing figure with a gruff manner.
But when he spots Randl, the palliative care co-ordinator, he turns into a flirt. "Are we going to see each other socially?" he asks her.
Miki has lived on the streets for most of his life, with various addictions. He's given up the methamphetamine and crack cocaine, but he can't give up the alcohol, still drinking up to 10 beers a day.
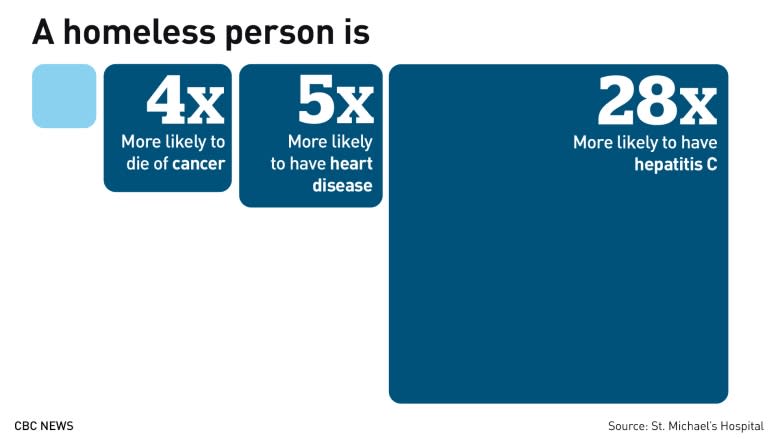
He's got cirrhosis of the liver and hepatitis C. The damage to his liver is irreversible, says Dosani.
"I put myself in this position years and years and years ago," says Miki.
Dosani knows he can't stop Miki from drinking, but he can try to lessen the liver damage by treating the symptoms, creating a safe place for Miki at the shelter and trying to improve the time he's got left.
"Palliative care is not a place," Dosani tells Miki. "It's an approach which we're trying to bring to you here. We're trying to give you the opportunity to feel as good as you can given what's going on."
Miki says he's "not long for this world."
"I woke up — and the rest of the day is going to be gravy."
Dosani leaves Miki and hopes to see him again in a few weeks. "He's vulnerable. He knows he's dying," he says.
"How do we value dignity at the end of life?" Dosani says. "Is it the same for everyone? My experience has shown it's not. It troubles me that we live in a society where we live differently. But should we really die differently?"
Palliative care 'a human right'
"Palliative care is a human right for everybody in Canada," says Dr. Simon Colgan, who set up a similar mobile medical service last October in Calgary, a city with about 900 people who are chronically homeless.
CAMPP, Calgary's Allied Mobile Palliative Program, is running with the help of a nurse and soon-to-run-out funding from the United Way.
"If there are some sections of our society that have difficulty accessing that care," Colgan says, "then I think we as leaders and as health care providers should find ways to navigate that system for them."