Use of opioid overdose antidote by paramedics jumps 222% in 1 year
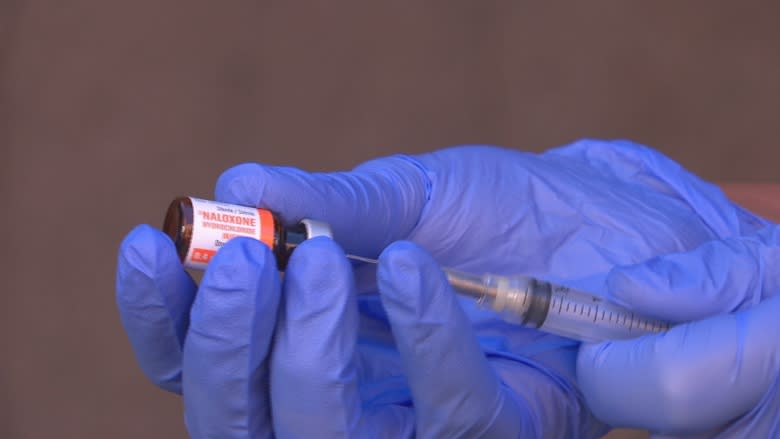
Paramedics at Ambulance New Brunswick are using naloxone more often, according to new data released through a right to information request.
It shows that paramedics have used the antidote to reverse an opioid overdose 77 times in the first three months of 2017.
That's a 222 per cent increase over the same three-month period last year.
Officials at Ambulance New Brunswick say that doesn't mean paramedics are necessarily seeing more overdoses.
Instead, the increase is likely due to a new policy that encourages paramedics to use the drug more often, according to Eric Beairsto, Ambulance New Brunswick's manager of training and quality assurance.
"You had to be really sure before you gave it," Beairsto said.
"We've opened that up quite a bit because it's a very safe drug. It's only not safe if you don't use it."
It means paramedics no longer wait for telltale opioid overdose signs such as a needle nearby or pinpoint pupils before administering the overdose antidote.
If a person is unresponsive with shallow breathing, they administer a dose of naloxone. If it's used successfully, it can jolt a person awake from a life-threatening overdose and buy paramedics crucial time to get a patient to the hospital.
A more powerful dose
Ambulance New Brunswick changed the policy in the fall after watchinga spate of opioid overdoses — caused mainly by a surge in illicit fentanyl — claiming thousands of lives in western Canada.
"We're forward-enough thinking that this past fall, after listening to the news and watching what's happening on the west coast, we thought, well, it's probably time to prepare [for] if it does come here," Beairsto said.
At the same time, the ambulance service also doubled the dose of naloxone being administered to patients, from 0.4 mg to 0.8 mg. Instead of waiting five minutes to administer a second dose, Beairsto said the wait is now only a couple of minutes.
Paramedics in places like Vancouver have reported that one dose is sometimes not enough to reverse the effects of an overdose from powerful opioids like fentanyl.
"So we're giving more of the drug and we're giving it more frequently," Beairsto said.
While paramedics have carried naloxone for more than a decade, the antidote is still not readily available for members of the general public, including harm reduction groups like AIDS Saint John.
Those people need to pay for kits out of pocket, something Nova Scotia's government is trying to eliminate by moving toward publicly funding naloxone for everyone.
Tracking fatal overdoses
At least four people have died in New Brunswick from accidental opioid overdoses so far in 2017. One of those overdoses involved fentanyl.
Last year, at least 23 people died from opioids accidentally, including three from fentanyl, according to numbers provided by public health.
But data from the coroner's office is often months to a year behind.
New Brunswick has now followed the lead of provinces like British Columbia, Alberta and Nova Scotia by tracking overdoses, including non-fatal ones, in close to real time.
That's done by collecting information on opioid overdoses from hospital emergency rooms weekly and from paramedics on a monthly basis.
It's then fed to public health, where an epidemiologist scans the information looking for trends.
Dr. Jennifer Russell, the province's acting chief medical officer of health, estimates that could trim the wait time down to one month from eight to 12 months.
"We know that having that information is really critical to making all the other decisions we have to make," she said.
Gaining access to those numbers as a member of the public is more challenging.
Ambulance New Brunswick would only provide overdose data to CBC News through a right to information request.
Russell said the public should "absolutely" have access to the numbers, but couldn't provide a timeline for when the data will start to be published online.
"We want to make sure it's clean data, that's it's very accurate, that it has been checked and counter-checked against the different sources to make sure we're not duplicating anything."
Horizon Health Network says it treated 13 patients for accidental opioid overdoses between March 1 and April 29 of this year.
Overdose death toll in B.C. rises
For the last year, a special group has worked to track opioid overdose deaths in real-time in British Columbia, which declared a public health emergency last year to deal with the overdose crisis.
That province has managed to take overdose tracking a step further by speeding up autopsies at the coroner's office, producing a weekly report on opioid overdose deaths.
In addition to coroner's office data, the group uses information from paramedics and hospital emergency rooms, where doctors document the drug a person thought they were taking and what drugs showed up in urine analysis.
It's helped officials target where and when to devote more resources to preventing overdose, according to Dr. Kanna Hayashi, a research scientist at the British Columbia Centre on Substance Use and a member of the tracking group.
"The rate of overdose death varies a lot by week," Hayashi said.
"For example, we noticed a spike in overdose deaths during the week of cheque day."
But real-time overdose tracking takes a lot of manpower and resources from the provincial government, Hayashi said.
And despite the work in B.C., the death toll is rising.
"Unfortunately, the number of opioid overdose deaths continue to climb, which is really, really devastating and disappointing," Hayashi said.
"Fentanyl-detected overdose deaths continue to rise. There's a lot more to be done."