Patients tell the inside story of Ontario's emergency rooms
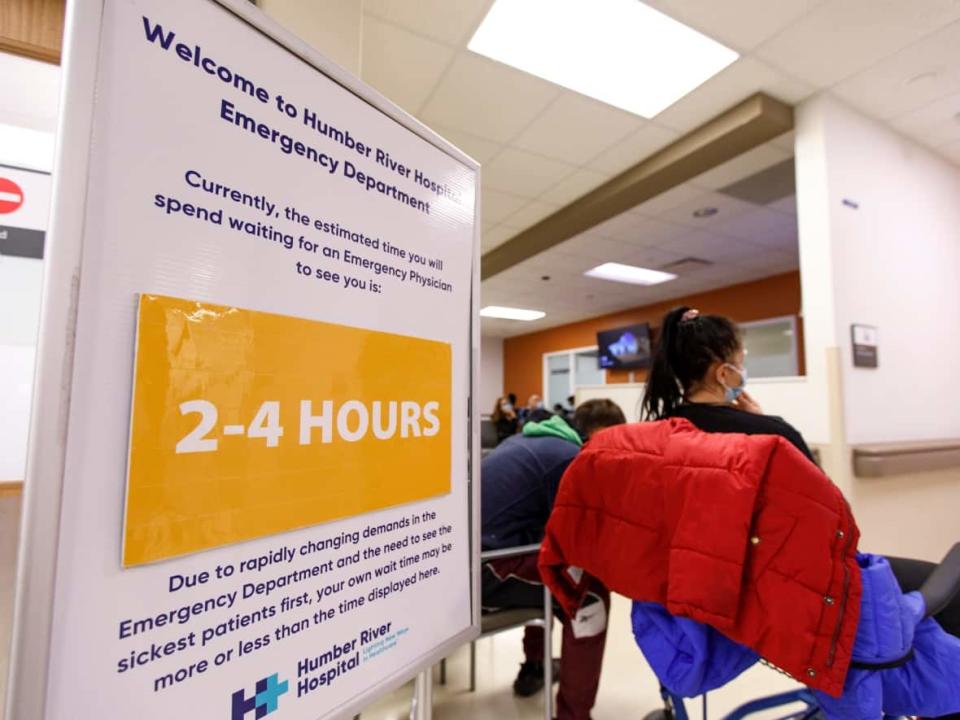
People who have visited a hospital emergency room in Ontario recently are describing their experiences of lengthy waits for treatment or to get a bed.
Their stories are part of the extraordinary trends seen in the province's hospitals over the past few months. Although spring is usually a time when the emergency departments are less backlogged, the latest statistics from Ontario Health show that wait times for ER patients to be admitted hitting all-time highs.
As previously detailed in reporting by CBC News, the record-setting ER bottlenecks are being caused by a variety of factors outside the emergency rooms, including a crunch in getting patients admitted because hospital wards are operating at or above full capacity, staffing shortages from COVID-19 exposures and burnout, and limited access to family doctors.
Dozens of patients and their family members reached out to CBC News to tell their emergency room stories. Here are a few of them.
Family doctor wouldn't see feverish child
When Mia Hutchinson took her daughter Téa to the emergency room at Sick Kids Hospital in Toronto on a Wednesday night in June, the board in the waiting room indicated a wait time of three-and-a-half hours.
"So we thought maybe four, four and a half hours. We never thought it would be eight hours," said Hutchinson.
"We sat in a hallway with three other families for about five hours, then moved to a room where we waited another three hours."

By the time the family made the decision to go to the emergency room, Téa had been running a fever of 39 to 40 degrees with a bad cough for four days, and had become dehydrated.
"We could not get the fever down. We called our family doctor and were not allowed to bring her in [to the doctor's office] because of her symptoms," said Hutchinson.
"When we call the doctor and are told because we are sick we can't come in, it makes no sense," she said. "Aren't doctors for the ill? Being refused to be seen caused us to go to the emergency room."
Hutchinson says she saw other children in the ER with high fever and cough, symptoms that she believes — like her daughter's — could have and should have been handled at a family doctor's office.
Cancer patient endures 3 lengthy waits in ER
Nancy Hunter says her husband Kevin received marvellous care from the staff on the cancer ward at Victoria Hospital in London, Ont., but his experiences in its emergency room were anything but ideal.
After Kevin's diagnosis of lymphoma, cancer ward staff issued him a special card with instructions that while undergoing chemotherapy, he should get to the ER immediately if a fever develops.

"They assured us that this 'fever card' would help the ER staff in identifying Kevin as a cancer patient," said Nancy. "The impression was we would be given priority. Our experience was completely the opposite: no priority given."
On his three visits to the hospital's emergency room over the course of two months last fall, his wait was never less than 10 hours.
"Each time we went to the hospital ER, our wait to even get a bed was painfully long," said Nancy. "Kevin was immune compromised from his cancer treatment, therefore our perceived risk created another level of anxiety."
During one wait in the emergency department, he vomited on the washroom floor, yet did not get a bed for several hours after that. Even arriving by ambulance on his third visited did not shorten the wait: he was not admitted for 13 hours.
Kevin Hunter died of lymphoma in November. The couple had been married for 47 years.
"I still don't understand why very ill cancer patients have to endure hours in any ER," said Nancy.
14 hours in a chair, 48-hour wait for a bed
On a Wednesday in mid-June, Fiona Hammett's blood pressure was dropping and she passed out. She was taken to the emergency room at Hamilton's Juravinski Hospital, where her son Greg Noonan says she waited 14 hours in a chair before she was seen.
"A nurse came to help her go to the washroom when she passed out again, she was showing signs of a stroke," said Noonan. "After 20 hours they told her she was being admitted and then offered her a stretcher to let her lay down."

Noonan emailed CBC News that Friday morning, 39 hours after Hammett arrived at the ER.
"She is still in emergency today on a stretcher because there are no beds available," he wrote. "This health system is broken. These nurses are overworked. Something needs to be done."
Hammett eventually got a bed on a ward at 8 p.m., after more than 48 hours in the emergency room, Noonan said. She stayed in hospital until being discharged in late June and she is now waiting for an MRI.
A broken bone, a long night in ER
Mona Romeh had been waiting in the emergency room at Oakville Trafalgar Memorial Hospital for nearly six hours with a broken bone in her right hand when she spotted this story about ER backlogs in Ontario, and sent an email to CBC News.
"Funny how I came across your article now. As I sit here. So fitting," Romeh wrote.

"I have not seen a doctor yet," she said. "I'm here for a broken bone requiring surgery and now I just may just leave. This is absolutely ridiculous. It's a horrible feeling, the ping pong back and forth of thoughts, do I stay, do I go?"
Romeh said she was feeling "frustrated and tired and just plain defeated" but also worried that leaving the ER would make her feel worse and risk damage.
She stayed, and took part in what she described as a large early-morning conversation about the current state of health care in Ontario among some of the patients and a group of nurses. "They were empathetic and were just trying to deal with the situation they were handed," said Romeh.
She was eventually seen by a doctor and was referred to Milton Hospital for surgery in late June.
'Something has to change'
On Father's Day, William Walker's blood pressure spiked. "He was feeling very dizzy, had a headache and was nauseous," said his wife Grace Walker. "He has a heart condition so we didn't want to take any chances."
She called Telehealth Ontario for advice and was told that William's symptoms warranted going to the emergency department. His wait at Lakeridge Health in Oshawa lasted nine hours.

"Something has to change when you see very young babies and the elderly waiting for hours to be seen by a doctor," said Grace.
She and her husband saw a lot of people in the ER with what appeared to be minor injuries such as sprained ankles.
"Surely some of them could have been taken care of at an after-hours clinic or waited until the next day to seek treatment," said Grace.
"At one point one of the nurses came to the waiting room to announce that there would be a three- to four-hour wait from here on and suggested some alternatives, like another hospital, urgent care or family doctor. No one moved."
A hip fracture at age 100
Irene Fraser has only been to an emergency room twice in her life, and that is all the more remarkable given she's 100 years old.
Fraser suffered a fall at her long-term care home on a Sunday in mid-June and was brought to the emergency room of Hamilton Health Sciences' Juravinski Hospital before noon. Her son Jim and daughter-in-law Janet Fraser, a retired registered nurse, say Irene was still in the hallway at 10 p.m., hadn't seen a doctor and was not permitted to drink anything.

"It seemed there was nothing that could be done for her until she was seen by a physician," said Janet, who took turns along with her husband staying with Irene.
"I wondered why they had not started an IV on her. I did tell the nurse at the desk that I was concerned that she had had nothing to drink all day and dehydration had been a problem for her in the past. She also was without her regular meds all day, as far as we know."
Janet says she knows how well-educated and capable nurses are, so she doesn't understand why tests and X-rays could not have been ordered by the emergency room RNs or nurse practitioners.
"The whole time we were there, no one had come to speak to us about her care, nor did anyone ask us about her health, her needs, her habits, cognitive abilities, her pain, her hearing or vision, health issues," said Janet.
"We could have provided much needed information."
Irene was seen after midnight by a doctor, who promptly called Jim with what he says was a kind and thorough explanation of the benefits and risks of surgery for her fractured hip.
She is now back in her long-term care home, recovering from the surgery and receiving physiotherapy.

