Why this woman credits 'liquid handcuffs' with saving her life
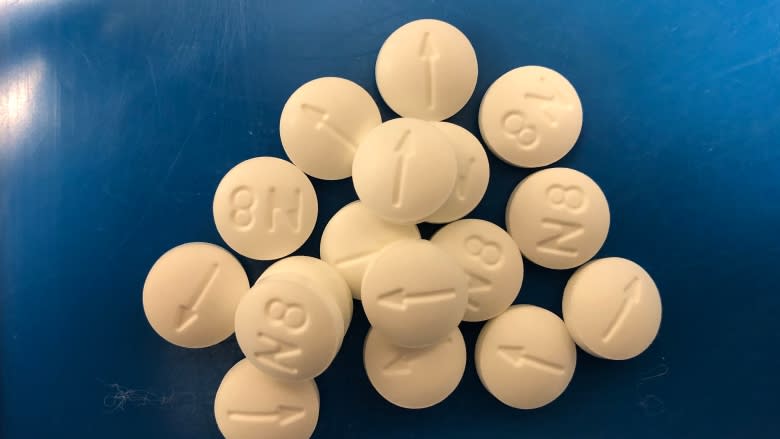
"Liquid handcuffs" is how Alyssa Francis describes her relationship with methadone.
She's tied to her daily dose to help her kick her dependency on opioids — a treatment that comes with regular pharmacy and physician check-ins, and testing to confirm she's not taking any other drugs.
"It saved my life," she says, with a wide grin. "I'm doing a lot better now. My health is better. I'm living at home with my mom. I'm pretty happy."
Francis' story begins like many of the roughly 1,100 Islanders who are currently battling an addiction to opioids.
The 25-year-old has struggled with medical issues — in her case intestinal problems — since she was born. She's undergone more than 50 surgeries over the years. She was prescribed drugs to handle the pain, and developed a dependency on hydromorphone, escalating to injecting drugs at the age of 17.
"I ended up being homeless and sleeping in a tent in the middle of the winter ... I went to jail," said Francis, adding that addiction "takes a lot out of you. It doesn't matter who you are, it'll take something from you."
Francis decided to regain control of her life, went through detox and started on methadone through the provincial addictions treatment program.
"It took a lot but I wanted to better myself so the only way I could be able to do that was with methadone."
Numbers on methadone, suboxone rising
In 2017, 1,094 Islanders were relying on methadone or suboxone to beat their addiction. The numbers have been rising steadily each year, up from 239 in 2010.
But as the numbers of those turning to opioid replacement therapy (ORT) rises, the number on opioid prescriptions has been steadily falling — from 19,355 in 2010 to 17,727 in 2017. Health officials take this as a sign that there are fewer people actively battling opioid addictions.
Transitioning to methadone isn't easy though. As Francis' body adjusted to the new drug, and the dosage was modified, there were side effects.
"You feel chills, shakes, the restless legs. You get sick. It's a process but you have to learn how to fight the cravings and fight those urges."
Through treatment and therapy she learned how to do that, and now she's back home, living with her mother Wendy.
'Saves a lot of lives'
Methadone and suboxone are criticized in some circles as just substituting one opioid for another.
But staying on methadone or suboxone for decades is better than the alternative, according to Dr. Peter Hooley, the medical director at the Queen Street Recovery Clinic, a private clinic in Charlottetown with six doctors monitoring patients.
"It's really a no-brainer ... going on opioid replacement saves a lot of lives," he said.
About half get hooked on opioids they started taking to deal with physical pain after accidents or surgeries, he said, with the other half escalating from recreational use to dependency on harder drugs.
The doctor said ORT reduces the risk of hepatitis and HIV, leads to better mental health, better chances of keeping a job, staying in school, and more solid connections to family and community.
It can cost up to $150 a day to support an illicit habit with street drugs, he said, which few can afford through legitimate means, so getting more people into treatment is also being credited with reduced criminal activity.
Weaning off methadone
Methadone was once considered a life-long replacement for those looking to kick their addiction to heavy-duty opioids like heroin, percocet and dilaudid.
But no longer. About 20 per cent of patients at the Queen Street Recovery Clinic in Charlottetown are in the process of being weaned off opioid replacements.
And of the 502 clients the clinic has seen since it opened in the fall of 2014, 22 have successfully gotten off methadone or suboxone and remained clean from all drugs for over a year.
Of the rest, 400 are still active patients, while the remainder quit the program, were asked to leave for failing to stay clean, transferred to other provinces, or landed in jail.
Relapses are common, said Hooley. "Addiction is a chronic illness."
While some patients do want to get off ORT eventually, others are functioning well on methadone or suboxone and don't want to risk losing that stability, said Hooley.
"I think a significant number of people are going to be on these drugs for life, and many of them will be on them for many years."
Hooley's numbers are for his private clinic in Charlottetown. Numbers from the provincially run clinics in Summerside and Montague and the treatment facility in Mount Herbert were requested by CBC News but not provided.
No wait list
It's relatively new territory. But slow and steady seems to be one key to successfully weaning off ORT, said Hooley.
Other positive influences are having a job or going to school, having stable mental health, and good supports of family and friends.
Chances of success are drastically reduced, said Hooley, for those who are living with or remain friends with those still taking drugs, those dealing with unmanaged pain, and high levels of stress.
Hooley believes P.E.I. has reached a plateau with illicit drug use.
His clinic is seeing fewer and fewer new clients struggling with addiction and he considers that a sign of the program's success.
At this time there is no wait list — a "massive improvement" from a few years ago when the system was overwhelmed by a flood of people looking to access treatment.
Move to suboxone
Methadone was the first big breakthrough treatment to address opioid problems. However as of last month, new Canadian protocols recommend suboxone as the first option in therapy and Hooley is now starting most new patients on suboxone instead of methadone. It is slightly more expensive, but is covered by the provincial drug plan and private insurance plans, he said.
"The main benefit to suboxone is safety," said Hooley, with less risk of overdose than methadone, less drug interaction and less stigma. Patients seem to tolerate the drug better, function better and stabilize faster, which he hopes will lead to greater success with sticking with it, and potentially eventually weaning off ORT.
Alyssa Francis always had a goal of weaning herself off methadone.
When she first started taking it, she thought she'd be finished in a year. But she soon realized that a five- to 10-year time frame was more realistic.
After two years of regular doses, her physician gradually began reducing her dosage. After a year, she's managed to cut it in half.
Her "liquid handcuffs" have loosened over time.
Those new to the program must visit the pharmacy every day and take their dose under the supervision of a pharmacist.
Over time, Francis graduated to weekly visits. She takes one dose at the pharmacy and carries six doses home in a locked box. She brings the empty bottles with her weekly when she replenishes her supply.
However, she continues to provide urine tests every four to six weeks at Mount Herbert Addictions Centre to confirm she isn't taking other drugs.
She's looking forward to being free of those restrictions and check-ins, and the ability to travel more.
"I want to continue getting off as soon as I can and as soon as my body's able to."
Her new goal is to be methadone-free in another year.
More P.E.I. News