How America’s Mental Health Crisis Became This Family’s Worst Nightmare

HIGH FALLS, N.Y. — The last time Emily Abramson saw Andy Neiman, he was in the waiting area of a hospital emergency department. She knew her brother was in trouble. But she figured he’d be safe.
It was before dawn on May 21, 2021, just a few hours after Emily had found Andy confused, agitated and running through an orchard adjacent to her house in a rural part of the Hudson River Valley. Andy had bipolar disorder, the psychiatric condition that causes dramatic, recurring bursts of euphoric mania and deep depression, and he was in the midst of what Emily and the rest of their family had come to recognize as one of his manic phases. The 47-year-old actor/playwright was speaking rapidly and disjointedly, though with more desperation than usual. He kept talking about a searing pain he felt under his skin — the result, he said, of toxins he had absorbed while staying in a cheap hotel — and was tearing off his clothes for relief.
But Emily believed Andy could get better, because he had gotten better before. The 20-plus years since his initial diagnosis included lengthy periods when medication and counseling allowed him to laugh, love and work. In 2012, he’d gotten married to a fellow thespian; in 2013, the two had a baby girl on whom he doted. He had picked up jobs waiting tables while appearing in local Shakespeare productions and making progress toward writing plays of his own. For these stretches, Andy was on his way to realizing the potential others had seen in him ever since he was an 8-year-old starring in a production of “Pinocchio” or when he was a champion performer on the high school debate circuit.
The first step, Emily knew, was to get Andy stabilizing care at a hospital. The closest was about 20 minutes away in Kingston, the historic small city on the western banks of the Hudson, but it had closed its psychiatric wing a year before. Emily’s husband began researching options online and suggested she take Andy downriver to MidHudson Regional Hospital in Poughkeepsie. It was a larger facility that still had inpatient psychiatric beds and likely where Kingston’s emergency room would have transferred him anyway.

The drive to Poughkeepsie was hillier and about twice as long. Emily can’t remember whether Andy sat in the front or back seat, but she recalls him talking much of the way, apologizing that he was a source of such trouble for her. People experiencing psychosis frequently lack “insight,” meaning they don’t realize they are sick or experiencing symptoms, but going to the hospital had actually been Andy’s idea — a promising sign, Emily remembers thinking. At the emergency department, she gently hugged him goodbye; COVID-era rules meant she couldn’t go with him. She consoled herself that he’d get the attention he needed once the hospital admitted him and put him in a room.
But Andy never got that far.
Hospital staff moved him to a specially secured part of the emergency department called the Monsignor Brinn Center for Psychiatric Care, which MidHudson opened in 2014 as a way, per its news release at the time, to provide an “enhanced patient experience” for “patients and their families in crisis.” Seven years later, many staff, therapists and families knew it simply as “the Brinn,” the place where patients ended up waiting for admission when inpatient rooms at MidHudson and surrounding hospitals were full. Which, according to former and current staff as well as patient advocates, happened so frequently it hardly seemed remarkable.
The hours went by — eight, ten, twelve. “I couldn’t believe how long it was taking,” Emily told me later. By late afternoon, Andy was calling Emily to say he didn’t want to stay there anymore and couldn’t understand why they wouldn’t let him go. At 9:06 p.m., some 16 hours after Emily had first brought Andy to the ER, she got a message from a hospital staff member saying they had found a room for him and would be admitting him sometime “in the evening.”
Less than 30 minutes later, Emily got another call. This time it was the police. Andy was gone.

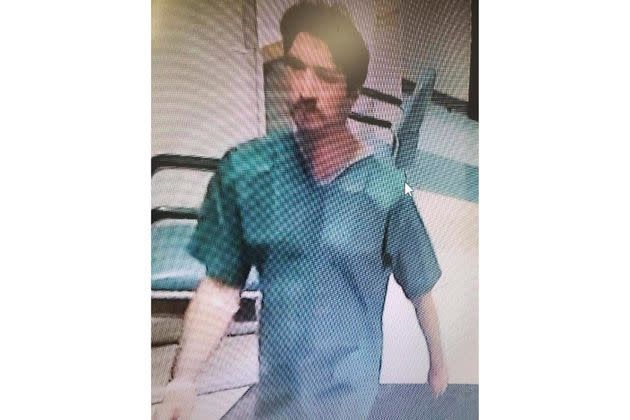
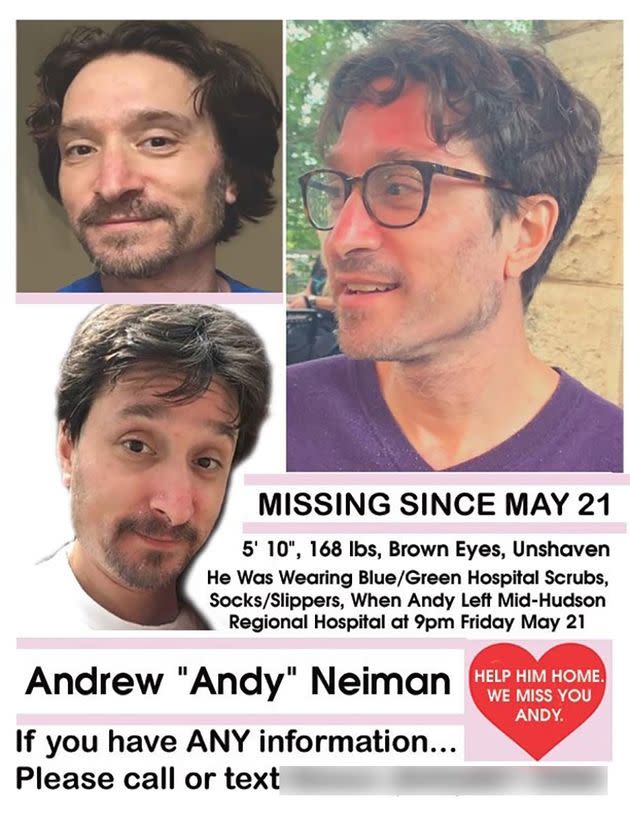
He had figured out how to leave the Brinn and then walked right through the main emergency room doors. He was wearing scrubs and slippers, security footage later revealed, and left behind both his reading glasses and phone. Emily hoped that meant he intended to return, but that hope faded quickly. “MY BROTHER IS MISSING,” Emily wrote two days later on a Facebook page her husband created to coordinate searches and help the police. “A part of me feels reluctant to make this so public but I am in such a state of worry and fear that I have to cast the net as wide as possible.”
The Facebook page picked up 2,000 followers, getting a boost when the Bravo television host Andy Cohen, who had gone to summer camp with Andy as a child, learned about the disappearance and started spreading the word. That led to a mention on NBC’s “Today” show and an article in People. “Missing” posters with Andy’s picture and description went up all over towns along the river. Soon the tips started pouring in. Somebody thought they spotted Andy underneath an overpass near the hospital, another at a diner. One person even thought they’d seen him more than a thousand miles away in Birmingham, Alabama.
But a month passed and still there were no signs of Andy. Then, one day, police reported the discovery of a body by the river. Decomposition suggested it had been there for some time, and police said they couldn’t even tell if it was a man or a woman. Then dental records confirmed the identity: It was Andy.
Nobody is really sure what happened to Andy after he left the hospital — or how he got out. Andy’s wife, from whom he had separated but remained close, filed a lawsuit against MidHudson on behalf of Andy’s estate alleging several acts of negligence — among them, “failing to implement security measures to prevent the elopement of an acutely psychotic patient.” The hospital’s parent company recently settled the lawsuit for $1 million without conceding responsibility or wrongdoing. It declined to comment on the case, citing patient privacy rules.
But whatever questions remain about the specifics of Andy’s care and disappearance, a few things are clear: Andy needed inpatient psychiatric care that day. He didn’t get it. And that was hardly an unusual occurrence.
Every day, all over America, people in psychiatric distress sit inside emergency departments — not just for hours, but frequently for days and sometimes for weeks. It’s happening in Massachusetts and Minnesota, Tennessee and Colorado, North Carolina and Iowa. The health care industry calls this “boarding,” and roughly 80% of hospitals regularly board psychiatric patients, according to survey data from the American College of Emergency Physicians. “This is not a one-off. This is not a situation where some areas are just greatly impacted and others are not,” the organization’s president, Aisha Terry, told me recently.
“I would actually refer to this as a public health emergency,” she said.
The proximate cause for all of these psychiatric patients in emergency departments is a relative dearth of available beds. But that shortage is really just the most visible symptom of a bigger, more fundamental problem: a failure to treat serious mental illness at earlier stages and a failure to surround the mentally ill with appropriate support. In other words, the reason ERs are packed with patients in psychiatric distress isn’t just that there are too few places to send them. It’s also that so many are arriving in the first place.
This is in some respects an old story. Mental health has never gotten the kind of attention, sympathy or resources that physical health does. But this familiar tale has a new, infuriating twist: The ability to recognize and treat psychiatric illness is better than ever.
Modern medications are more effective at controlling symptoms and less likely to produce side effects. Newer strategies, including assistance finding employment and housing, hold the promise of allowing people with serious mental illness to engage in society more fully. And if these strategies don’t work for everyone — serious mental illness remains, in so many ways, the most difficult disease for science to tackle — treatment has come a long way since the days when standard regimen included lobotomies, removing organs or locking patients in asylums.
But to benefit from modern psychiatric care, people need to get it. For millions, that doesn’t happen on a regular basis, if it happens at all. Calculations from the Substance Abuse and Mental Health Services Administration suggest that about 1 in 3 Americans with serious mood or anxiety disorders don’t get treatment. While sometimes it’s because they don’t have insurance — another familiar, if uniquely American, story — other times it’s because they simply can’t find providers, facilities or programs with the capacity to handle them.
The effects reverberate through society in ways that can be measured with aggregate statistics, like the number of people living on the streets or the amount of money funding jails that have become de facto asylums. But the impact is probably most vivid in the individual lives it affects.
There are the high-profile stories of catastrophe, including deadly encounters with police, violent crimes and suicides. There are many more instances when people with untreated mental illness are simply unable to function or to participate fully in everyday life.
And then there are the stories like Andy Neiman’s.

It is a warm-ish day in early May. Emily is sitting on a lawn chair outside her weathered, light blue home, near a pair of large flowering shrubs and a few steps away from the orchard where Andy went running that night three years ago. Their mother, Lainie Neiman, is there too. A few minutes later, their brother, David Neiman, arrives by car.
I’ve spoken with all three at length before but only individually. It’s a more lively experience speaking with them together, when they are frequently interrupting or talking over one another; at one point, Lainie was simultaneously telling me a story about Andy’s childhood and arguing with David about whether her old Peugeot sedan was maroon or blue. It doesn’t take long to imagine how conversations like these must have unfolded when Andy was there and at his sharpest — or to understand why a richly rendered portrait of Andy that ran in a hometown publication called the Riverfront Times likened him to a “comet flashing through the darkness.”
Andrew Michael Neiman was born in St. Louis, Missouri, in 1973. He was the oldest of his three siblings and he was, according to Lainie, precocious from the very beginning. Two relatives who saw Andy in the hospital nursery told Lainie that he was already trying to lift up his head, something babies can’t actually do until they are several weeks old. He had a discernible sense of humor by the time he was 2, Lainie said, and was so extroverted he’d greet every passerby in the supermarket while she pushed him in the cart. If they didn’t answer, Lainie said, he’d keep at it — “I said hiiiiiii” — until they responded.


Growing up, Andy’s confidence and enthusiasm attracted lots of friends — boys and girls, younger and older. He loved to perform, and he craved an audience. Later his family would think back to a comment he made while Lainie was driving him home from his turn at Pinocchio: “Mom,” he said with a sigh, “I really hate when the applause stops.”
In high school, Andy started taking the craft more seriously and joined the debate team, winning state championships in both dramatic and humorous interpretation. He also won a Bronfman Fellowship — a highly selective nationwide program that allows students to spend several weeks in Washington and in Israel, meeting with Jews of different denominations to explore and discuss the meaning of their faith.
Lainie said it’s hard to be sure when the first signs of a serious psychiatric condition appeared. She has a master’s in counseling and told me she recognized signs of attention deficit disorder when Andy was in middle school, though the symptoms were mild and basically under control with some minor changes in diet and rest. And while Andy had long bursts of energy that would carry him through the day, she said, that was very much what made him … Andy. “His mind never shut down, except when he was sleeping,” Lainie said. She likened him to a “wind-up toy” that would suddenly stop when he hit the pillow.

In adolescence, Andy’s family told me, they noticed him starting to keep more distance from his peers. “He had a lot of friends,” Lainie said, “but I think Andy always felt a little like a Martian. … He always felt different.” As one of four students to speak at graduation, he talked about his work on the video yearbook, focusing on what it was like to observe his classmates through a camera rather than to be with them. Andy was also struggling with problems in his personal life, including his parents’ divorce and what his family members described to me as a troubled relationship with a mentor. It left him “with a lot of unprocessed trauma,” according to Emily.
Andy’s struggles became more apparent at Wesleyan University, where, after three years of getting high grades and performing in several plays, he fell into depression. “I visited him and he was basically a disaster,” David said. Andy managed to graduate with his GPA intact and came back to St. Louis for the summer, where he was still stuck in a depression until one evening, in an emotional conversation with David, he suddenly became energized, started talking rapidly and insisted the two stay up all night — relenting only at 4 a.m., when David said he couldn’t keep his eyes open anymore.
David said he woke two hours later to see Andy looming over him, ready to start up the conversation again. Later that afternoon, after returning from a summer camp where he was working, Andy announced that he was taking the car because Newt Gingrich, the newly confirmed Republican speaker of the House, was appearing at a conference downtown. Gingrich was secretly gay, Andy explained, and it was time to tell the world. David said that when he questioned all of this, Andy grabbed him by the arm and took him around the house, explaining the “prophetic meaning” of every framed picture or artwork. “What are you saying?” David recalled asking, before Andy pulled him in close and said, “David, I am the messiah, and you and Emily are my prophets.”
David told their mom, who contacted Andy’s therapist. They all went down to the convention center, intercepting Andy just as he was talking his way inside. David, then a teenager, still didn’t know exactly what was going on with his brother. “He was so brilliant and so articulate, I was like, ‘Tell me more — and, also, this is a little crazy.’” Lainie realized that Andy’s delusions were likely a form of psychosis, the kind related to some kind of underlying disorder. He needed medical attention.

Andy was lucky that day, and not just because his mother had formal training in mental health. Her job was at a nearby hospital, where she worked on marketing for the psychiatric department, and she was able to take him there. “All these nurses and all these caretakers knew me and loved Andy,” Lainie said. “I’d have janitors coming up to me, saying, ‘We’re praying for your son, Mrs. Neiman.’” Administrators extended their own form of consideration, allowing Andy to stay for two lengthy stints — one for five weeks, one for three — and then writing off some $30,000 in charges when Lainie’s insurance carrier said Andy had exhausted the policy’s benefits.
This was 1995, a time when insurers could still have separate, tighter limits for mental health care coverage. Bipartisan federal legislation would later put an end to that practice. But the impulse to squeeze mental health care spending was part of a broader transformation already underway: the managed care revolution, in which private insurers became more aggressive about limiting treatments and access to specialists.
The idea was to reduce waste, reward efficiency and promote quality care, and in some instances it did just that. But the inherently subjective diagnosis and unproven treatment regimens of mental health care made it especially easy to tighten spending in ways that frequently seemed unrelated to — or even at odds with — better quality care, whether it was by second-guessing seemingly sound decisions from clinicians or keeping payments to the providers of care lower than in other medical fields.
The shift was clear to anybody with close exposure to the world of psychiatric care, and that included Lainie. “The entire health care system in this country was changing,” she told me.
It was only a matter of time before the changes touched Andy’s care too.
A constant challenge with mental health care is finding the right cocktail of drugs. It was an even bigger challenge in the 1990s, when Andy had his first psychotic break and got the diagnosis of bipolar disorder, because treatments were more rudimentary than they are now. Doctors tried multiple combinations of medications, typically mixing antidepressants with “stabilizers” designed to prevent manic episodes. All could have significant side effects — rapid weight gain, involuntary physical movements, overall sluggishness — that made patients like Andy reluctant to take them.
“He was taking lithium, Risperdal, Stelazine, Ativan — these drugs would strip him of personality; you could literally see it in his face,” David said. “There would be moments where he would literally just put the pill bottle down, because … he needed to have that feeling again of being a person. And of course it would go further than it should have. He would have a joyride and then he would crash down into bedrock.”
Then, sometime around 2006, doctors tried Seroquel, a drug that the Food and Drug Administration would soon approve for schizophrenia and bipolar disorder. His family felt like the old Andy was back — “we were like, fucking hallelujah,” David said — as Andy got more acting work and focused more on writing too. He also reconnected with an actor named Louise Edwards he’d met in a Shakespeare company years before. The two married, settled in the Chicago area and had their baby girl.

“We were in Evanston at the time,” Louise said, recalling the first months after their daughter was born. “I was taking graduate classes at Northwestern, he was working in restaurants, and we were tag-teaming. … I remember she decided she wouldn’t take a bottle, so he would stick her in this sleeping bag thing we had in the stroller, and he’d just stroll her up to campus from the southern part of Evanston.”
Later they moved to St. Louis, near their families, and Andy turned into a host — cooking pies and mixing cocktails for groups of friends. Part of the routine was having the guests read bedtime stories to their daughter. “We called it our St. Louis reader series,” Louise said. “We had all these photos of all these people sitting down and reading books to our little girl. … He just loved people so much.”
Not that life was easy. Seroquel, like many psychiatric medications, requires regular monitoring and blood tests — and the full treatment regimen includes regular counseling. But finding therapists was difficult, Louise said, because so many wouldn’t take their insurance plan and provider network listings were frequently changing. “You’re spending all your time trying to call people to confirm, do you actually take this insurance? Are you actually taking new patients?” When they did find one, Louise added, Andy was on the hook for significant out-of-pocket costs.
“He was conscious of how expensive it was,” Louise said, and sometimes he spaced out counseling appointments to save money. Louise thinks Andy not seeing a therapist more regularly may have been among the reasons that, in 2019, they were slow to recognize that the Seroquel was becoming less effective. “It can be difficult to know how much help somebody needs until, all of a sudden, you’re in a crisis situation,” Louise told me.

Then the pandemic hit, taking away Andy’s drama work and the constant social interactions on which he seemed to feed. He became severely depressed and began talking about whether he thought his life was worth living. “He said this is a torture chamber, that this is a nightmare just living,” Emily said.
To this day, Andy’s family members wonder how much of his deterioration was because the medication simply stopped working, as psychiatric drugs sometimes do, and how much was the emotional shock of the pandemic and its effect on everyday life. Either way, the deterioration of his condition helped to unravel his marriage. He and Louise began living separately, and a few months later, he took a large quantity of pills and alcohol in an apparent suicide attempt. Once again, he needed some kind of intensive care, starting with a hospital. The question was where.

In the pre-Seroquel days, Lainie had frequently been the one to manage his care, because her background meant she had the contacts — and knowledge — to navigate the system in St. Louis. But she had now retired, as had most of her former colleagues. Andy’s siblings started taking on more of the work, as did Louise, even though she and Andy had separated. But the system they encountered was a lot less supportive than the one that had existed in the 1990s. An emergency room visit might lead to admission if he was in sufficiently dire condition, but doctors would inevitably discharge him after a day or two, declaring him stable enough — either because they believed he was or because insurers wouldn’t pay for a longer stay.
The search for a program that would keep Andy long enough to get on a better treatment course played out over phone calls and long chains of text messages. “Everybody was like, I’m going to research these places. OK, I’m going to research those places. I’m going to talk to this person and I’m going to talk to that person. OK, let me talk to the insurance company,” Louise recalled.
But trying to find a place that met all of Andy’s needs “was like fucking bingo,” David said. “They had to take our insurance, which eliminated so many. And whatever the deductible was, that would eliminate a couple more. And then we had to see if they were the type of facility that could take him based on the type of condition that he had.”
Even more baffling to the family, many facilities wouldn’t take Andy because of his recent suicide attempt. “These places are telling me, no, your brother’s not well enough to be here,” Emily said, “and I’m saying, I’m pretty sure the whole purpose of your program is for people who are deeply, chronically unwell.”
Andy’s treatment journey took him across the country — starting in Arizona (where he was accepted into a facility and then left because he was so unhappy with the care) and then to Texas (where he was briefly with his father before disappearing for a day). After that, David took him to a program in Pennsylvania, although at the drop-off Andy made clear it wasn’t such a great prospect either.
“I said, ‘It’s going to be OK,’” David recalled. “He said something about how ‘It’s very sweet of you to believe that,’ like ‘I really appreciate your faith’ — in a way that was very clearly, ‘You’re wrong. … I hate to tell you that it’s not going to work out for me.’”

Sure enough, Andy lasted there less than three days. It was a voluntary unit and Andy signed himself out; cigarette smoke from the substance abuse patients was contaminating him, he said. That is when he made his way to Emily’s house in New York, with the help of a credit card Louise was still paying and telephone conversations with Emily on how to find a hotel or how to buy a bus ticket. “Basically, I was coaching him every few hours on how to exist in the world,” Emily said.
She guided him to a train that deposited him an hour from her house — and was taken aback at how he appeared. “I hadn’t seen him in a year and a half,” Emily said, “and he was like a broken man, just sort of hunched.” He was complaining about physical pain, something that had started months before but was now worse, he told her, because of toxins he picked up at one of the hotels. In the car, Emily said, she reached out to hold his hand and he yanked it back. “I’m sorry, just every sensation is too much. I can’t do it,” she remembers him saying.
Still, she remained hopeful. She had already been thinking of how to set up care for him back home and thought that by staying with her, in her quiet part of New York, he might finally get the support he needed.
It was a reasonable bet, for a reason that Emily didn’t even know: New York has always been among the states to take treatment of mental illness most seriously.
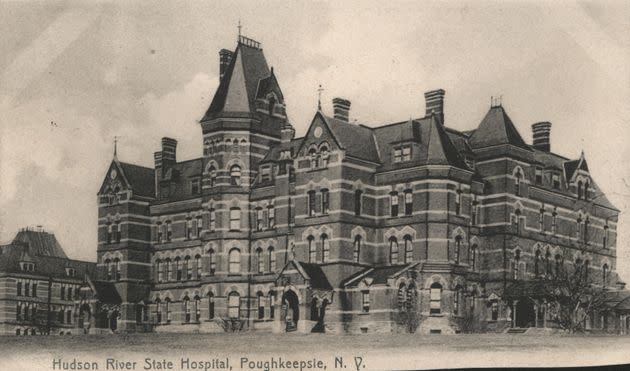
In the 19th century, the state was a leader in the asylum movement, which called on governments and philanthropists to build large institutions that for the first time would treat the “insane” not as criminals or demons but as people deserving of care. The idea of these asylums was to give people with mental illness a chance to get away from stresses of everyday life in order to create a sense of calm.
A by-product of that thinking was the Hudson River State Hospital, which opened in 1871 on a sprawling, wooded 300-acre expanse of Poughkeepsie hillside. It immediately won praise for its state-of-the-art buildings and care, and it remained the backbone of mental health care in the region for the better part of a century. In the 1950s, its inpatient population peaked at more than 6,000.
But by then, a dramatic change in psychiatric care was underway.
The introduction of Thorazine, the first drug that effectively controlled the most visible schizophrenia symptoms, sparked a push to minimize and eventually to empty these facilities. In the U.S., President John F. Kennedy formally launched this era of “deinstitutionalization” when he signed a landmark act designed to fund programs that would help the mentally ill to live on their own or with minimal help. Over the next six decades, the nation’s inpatient psychiatric population would drop from more than half a million to barely 100,000. Hudson River State Hospital’s patient roster dwindled apace until 2003, when its last patients left.
Nobody mourns the end of these institutions, which had come to resemble warehouses more than places of treatment. “You obviously don’t want a situation where you go back to the 1950s and you’re doing lobotomies on people, or just prescribing Haldol to everybody and people just walk around drugged out like zombies,” said Ryan McBain, a senior policy researcher at the RAND Corporation who has done some of the most authoritative work on psychiatric bed availability.
New York in particular had been rocked by a 1972 television exposé, put together by a then-low-profile local correspondent named Geraldo Rivera, uncovering abuse and neglect inside an institution for developmentally disabled children. And New York at times invested in the sort of community infrastructure that was supposed to take the place of the old asylums — everything from housing to job training to “partial hospitalization” programs that allowed people in distress to get intensive care while living on the outside. Many of these programs remain a pillar of the state mental health system today.
But federal funding to bolster these efforts didn’t last. A particularly crushing blow came in 1981, when Ronald Reagan effectively killed an ambitious community mental health program that his predecessor in the White House, Jimmy Carter, had signed. Even New York’s financial commitment proved inconsistent. During the 1990s and early 2000s, Republican Gov. George Pataki vetoed major mental health spending initiatives. From 2000 to 2018, the state ratcheted down payments to hospitals so that net revenue for each patient bed declined (adjusted for inflation) from $99,000 to $88,000 a year, according to an investigation that appeared in The River, a Hudson Valley news publication.

Deinstitutionalization “was started as a scientific and a social movement, to get people out of the hospital, but then it was also then taken over by fiscal conservatives as a way to save money,” said Jon Berlin, a former president of the American Association for Emergency Psychiatry and a highly cited researcher on the subject. “The money never followed those patients into the community, where it was needed for support, for the wraparound services or intensive outpatient treatment.”
With public funding in such short supply, programs have struggled to keep up with demand or, in some instances, just to keep their doors open. It’s still that way. In Dutchess and Ulster counties, which straddle the river and include Poughkeepsie and Kingston, respectively, people who run or work with community programs told me repeatedly they aren’t even close to meeting the demand for services that deinstitutionalization created.
Andrew O’Grady, chief executive of Mental Health America of Dutchess County, told me that case managers at his nonprofit agency would ideally have 20 to 25 clients because of their high needs and the attention each one requires. The actual caseloads are about twice that, he said. “People cannot get the level of care they need,” O’Grady said. “It’s just not available.”
The same thing is happening all over America, creating an even greater demand for stabilization and crisis services, which inevitably puts an even greater strain on hospitals to provide short-term, stabilizing care. But hospitals themselves are reducing capacity, in no small part because the combination of thin public funding and low private payments means psychiatric wings are a drag on the bottom line. And that’s before taking into account the costs associated with paying workers for what can be difficult work with patients who may not want treatment — and may even act out physically.
“The liability for having a psychiatric ward is very high,” O’Grady said. “Staff get injured all the time. That’s a lot of money in workman’s comp — it’s an expensive proposition with not the right reimbursement, so they don’t want to open more beds.”
On top of that, simply finding workers has become a challenge, according to Jean-Marie Niebuhr, deputy mental health commissioner in Dutchess.
“There’s not a lot of people and not a lot of entities throwing their hat in the ring to say, ‘Hey, I want to run an inpatient psychiatric unit,’” Neibuhr told me in an interview from her office in Poughkeepsie. “The staffing requirements are significant. There’s a major shortage in psychiatric providers. It’s really hard now even to get social workers, so there’s a lot of challenges in terms of operating this service. I’m grateful that we have a hospital right across the street here.”
When Neibuhr said that, she was talking about MidHudson Regional Hospital, where Andy went. It is part of the Westchester Medical Center health group, a nonprofit network that state officials have recruited over the past decade to take over several financially struggling facilities.
WMC executives say improving mental health care for the region has been a priority, citing as proof their support for outpatient programs and the creation of the Brinn at MidHudson. They are also quick to point out that their local competitors don’t even have full-fledged psychiatric wings anymore.
“In the Hudson Valley and across the country there is more demand for inpatient psychiatric services than there are beds available, recruiting and retaining nurses and physicians is a challenge and there is a national shortage of these specialists across the country,” a medical center spokesperson wrote in an email response to questions from HuffPost. “Despite this, our focus continues to be on how we can best serve the needs of our community, investing in and expanding psychiatric services instead of retreating from the space as others have done, and prioritizing keeping care as close to home as possible.”
Many local officials take a dimmer view of WMC’s record, pointing in particular to its management of the Kingston hospitals — the ones closest to where Emily lived and which before March 2020 had 40 inpatient psychiatric beds plus another 20 for substance abuse treatment. WMC shut them down following an order from then-Gov. Andrew Cuomo to create surge capacity for COVID-19 patients. Among those alarmed by the closure was Pat Ryan, who at the time was the area’s county executive and is now serving in the U.S. House. In May 2020, Ryan wrote a letter to Westchester warning that “loss of these beds would be devastating” and urging the company to once again make them available to psychiatric patients.
State lawmakers from the area issued appeals of their own. The Service Employees International Union and New York State Nurses Association did the same. But as negotiations between officials and WMC proceeded with no firm commitment to reopen the beds, critics said that the hospital network was, as Ryan put it to me in a recent interview, using “the cover of the pandemic to remove these beds, knowing that they’re never going to bring them back.”

The WMC spokesperson said “it is not accurate to say the plan was not to return inpatient behavioral health beds.” He also pointed out that the company immediately added 15 beds to MidHudson in order to increase capacity there. But whatever WMC’s long-term plan, the result of its decision was 25 fewer psychiatric beds in the area — and none at all in Kingston. “We palpably feel the loss of beds here,” said Tara McDonald, Ulster’s mental health commissioner.
At MidHudson, the mismatch between the demand for services and supply of hospital beds means that long waits for admission are now routine, according to multiple sources. “A lot of times, patients have been down in the emergency room for three to four days,” one MidHudson employee told me, asking not to be identified because they feared retaliation. “We rarely get a patient [admitted to psychiatric inpatient wards] that’s been down there less than 24 hours.”
“They spend at least a night, but most of them are spending three or four, possibly five or six days in the ER waiting for a bed,” said a worker at a Hudson Valley nonprofit agency who also asked for anonymity because they weren’t authorized to speak for the organization. “People might not think about it, just the experiences these people are having in the emergency rooms or the hospitals, but there’s a lot of trauma there that could be triggering for a lot of people to be in these places. And the longer that they’re there, the longer that they’re potentially kept in this state of crisis.”
People cannot get the level of care they need. It’s just not available.Andrew O’Grady, chief executive of Mental Health America Dutchess County
Sometimes the only way to find a bed is to go somewhere else: MidHudson ends up transferring 22% of its psychiatric patients to other hospitals, according to the WMC spokesperson. Most go to the system’s main hospital in Valhalla, which is about 50 miles away, or more than an hour’s drive even in good traffic conditions. Others have to go farther.
“I’ve sent people to as far as New York City or as far as Binghamton,” O’Grady said. “I’ve sent people four or five hours away for inpatient stays in an ambulance.” This can be tough on families — “imagine having your child go somewhere four or five hours away,” he said — and can make it difficult to arrange local follow-up care, even if it’s available.
Once patients do get admitted, local sources told me, the pressure to keep stays short makes it difficult to get patients the care that could actually help them.
“So you string together a day or two, where you haven’t screamed or yelled or acted weird, then ‘you’re OK to go home now’ and they discharge you — and you never get the care you need,” O’Grady said. “They hook you up with some basic drug, like Thorazine, and they try to hook you up with services in the community. There’s a nice program where a hospital might work with an agency like mine, and we get somebody in there to meet the person in the hospital and then we work with them when they get out. But that’s rare.”
WMC declined to provide specific figures on wait times. But its spokesperson said that providing psychiatric care brings multiple financial challenges, including “the uniquely complex and ongoing care requirements of individuals suffering from chronic severe mental illness compared to those who require hospitalization for primarily medical needs” as well as “gaps in community supports.”
The crowding is certainly a nationwide phenomenon, and sometimes the delays are mind-boggling. A 2022 report from the American College of Emergency Physicians featured accounts from anonymous members on the front lines, including one from a physician who wrote that “we held a 14 yr old girl in a tiny ED room for 42 days (!!!) awaiting transfer/placement for inpatient psychiatric care.” Another said, “I’m working in a 9-bed ED with an additional 3-beds dedicated to psychiatric patients. We now have a patient who has been boarding with us for over 5 MONTHS with no end in sight.”
In reporting this article, and canvassing for input from around the country, I heard repeatedly what this feels like for patients and their families.
One account came from an Iowa woman who said she’d been diagnosed with schizoaffective disorder and obsessive-compulsive disorder. She told me about multiple emergency room stays that spanned several days, inflaming her OCD because she became so worried about hygiene after three days without a shower. A Georgia woman said her younger brother has had multiple emergency room visits while in psychosis, only to get released after 24 to 48 hours because there was nowhere to admit or transfer him. “He comes out of the emergency room and he’s still completely delusional. He needs hospitalization and we’re back to square one, scrambling to find him help,” she said.
I also heard from a woman in the Poughkeepsie-Kingston area after she took her son to MidHudson: “The social worker sees him and I hear, within about three hours, that he’s been admitted and we’re calling all over for beds. … We’re calling to Sharon, Connecticut, we’re calling to Columbia-Presbyterian in New York.”

She described the room in the MidHudson psychiatric emergency department. “There’s a rocking chair that you can barely budge … and a bed and that’s it. Not a table or a place to eat a meal for instance.” She said her son had to wear only “paper-thin” scrubs with only underpants underneath. “When I visited, he’d sit at the edge of the bed,” she told me. “He couldn’t stay there for more than a few minutes before he’d have to get under the covers, because he was freezing.”
She said she understood (as the WMC spokesperson confirmed) that the requirements were safety protocols, designed to prevent patients from harming others or themselves. “If it’d been for five hours, 10 hours, that’s one thing,” she said. “He was there four days.”
As for Andy Neiman, the details of his evening at MidHudson are still murky.
The most concrete information I could find was from the lawsuit, via a deposition by the psychiatrist who was on duty that day. Andy got two mental health assessments, according to that deposition ― the first at around 7 a.m. from a social worker, the second at around 11 a.m. from a psychiatrist at another WMC hospital who met with Andy via video. These “telehealth” consults in the hospital have become increasingly common, either because hospitals can’t find psychiatrists to staff wards continuously, because telehealth is cheaper or some combination of the two.
Andy was in the Brinn for most of this time, the testifying psychiatrist said, before confirming that it was designed to be a secure space with just one entrance in and out. She said she didn’t recall seeing Andy, or thinking it was necessary, because the diagnosis and observations were already in the record: Andy had delusions and recent suicidal ideation, and had said “I’m feeling very scared.” He needed to be on the inpatient ward.
The lawsuit against MidHudson focused mostly on issues like whether the hospital had provided Andy with a one-on-one observer while he was waiting, what kind of security provisions the hospital had installed at the Brinn, and so on. But during the deposition, John Fisher, the lawyer representing Louise and Andy’s estate, asked the psychiatrist why Andy never made it to a room and whether one was even available. The psychiatrist, who had signed the admission order at around 5 p.m., said she didn’t know.
Fisher, who specializes in malpractice cases involving mental illness, thinks all of the signs point in one direction: “This was an emergency psychiatric situation of a patient who we contend desperately needed treatment and simply did not receive it.”
Emily described the weeks after Andy’s disappearance as the “most exquisite brand of torture.”
“I’d have that sort of peaceful feeling you get when you first wake up, and then I remember what the reality was and I’d feel like it was a nightmare. Like a sinking fear. And then I would feel that for much of the day.” She said she would scream and cry on her drive into work as a high school teacher, trying to steel herself before facing a classroom full of teenagers.
But as time passed, she and her brother thought Andy might be OK — that he was out there somewhere, in his “messianic” manic phase, proselytizing to strangers. They hired a private investigator, paying for him with the help of a GoFundMe that raised more than $65,000, and coordinated searches through wooded areas and along the riverbanks, even using drones.
It was David who first learned about the body discovery when he heard from a reporter who’d seen a posting about it on a Poughkeepsie Police Department web page. He called, told the police where to find dental records and pushed them to determine a match quickly.


When Emily learned her brother was dead, she continued to wonder if he had been trying to make some kind of spiritual journey. There were no signs of a fall, according to the medical examiner, or reason to believe he had tried to kill himself. Maybe he had been trying to cleanse himself in the waters, she said to me later, and somehow got himself caught on rocks. Or maybe — as David later speculated — Andy was trying to find his way back to Emily’s and succumbed to the currents while trying to cross the river.
The news of Andy’s death made headlines up and down the Hudson Valley, and advocates used it to strengthen their case for more beds. “It brought into such stark, real human terms what the cost of this broken system means … just every heartbreaking detail of it,” said Ryan, the county executive-turned-Democratic congressman. “It was just kind of this perfect storm that encapsulated all of that failure.”
One year later, following local media coverage and pressure from unions representing hospital workers, WMC announced plans to put 20 beds in the Kingston hospital, inside of a newly renovated wing. That was originally supposed to happen a year ago. Now the schedule calls for opening the beds in 2025 amid an ongoing dispute with state officials over funding. The WMC spokesperson stressed that the opening — and the addition of five beds to MidHudson — remain in their plans.
Other efforts to bolster psychiatric care in New York are further along. Kathy Hochul, the Democratic governor, has made mental health a priority since taking office in 2021 — and, working with the Legislature, she has delivered some concrete changes.
That includes a new law mandating that private insurers pay community providers at the same rate that Medicaid does. (Typically they pay less.) “It’s still not equal to what they pay for physical health care, but it’s an increase that we are hoping will lead to more providers taking private insurance,” said Matthew Shapiro, senior director for government affairs at New York’s chapter for the National Alliance on Mental Illness. Shapiro told me the group is now pushing to expand the rule so that it also covers payments to hospitals. “Hopefully that could be a generator for bringing hospital units back online.”
There’s also new state money in the pipeline, some of it already flowing and underwriting programs like 24/7 crisis intake centers where people in distress can go for assessments — and then either basic care or referrals to hospitals.
The policy action on mental health care isn’t confined to New York. In California, Democratic Gov. Gavin Newsom has pushed through what he calls “a major overhaul” of his state’s mental health system, including both significant new funding as well as new (and controversial) rules that make involuntary commitment easier.
At the federal level, Congress in 2022 set aside $8 billion to create networks of comprehensive mental health clinics. The law’s co-architect, Sen. Debbie Stabenow (D-Mich.), called it “the biggest investment in mental health and addiction services ever” — an assessment that might be correct. Next up may be a bipartisan proposal to alter a rule that effectively limits what Medicaid pays for inpatient psychiatric care. The proposal has support from high-profile organizations such as NAMI and the Treatment Advocacy Center.
Are there any other emergency medical conditions — heart attacks, sepsis, broken bones, anything else — where we tell people just to wait until there’s a bed somewhere?Jon Berlin, former president of the American Association for Emergency Psychiatry
Just how well the new investments pay off is to be determined. In New York, social workers and local agency heads told me they worry about the rules that come with some of the appropriations. O’Grady cited as an example the paperwork for each client that the state requires, making it even harder to give each person the time they need.
O’Grady also has concerns about a requirement in a highly touted new housing initiative. It prioritizes the patients in the worst condition who, O’Grady explained, may also be the ones least able to make a go of independent or partially supervised living. That could lead to a higher failure rate, making the program’s funding difficult to justify in future budget negotiations. “It doesn’t make sense to me,” he said.
But lack of money is still the primary issue, several advocates said, because the history of underfunding goes back so far. “We’re really trying to dig ourselves out of a massive hole,” Shapiro said, after praising Hochul and her allies for what they have done in the past three years. “There’s been limited investments in mental health care for decades, really since deinstitutionalization, that’s led to this situation.”
Finding the money to meet America’s mental health needs would inevitably require the same kind of political spadework and dealmaking that any such initiative would. But it may also require a broader change in American culture and understanding. It is true that psychiatric illness doesn’t carry the kind of stigma it did a century or even a decade ago. It is also true that it is still not seen as an affliction in the same way that physical ailments are — a point that Berlin, the psychiatrist and researcher, emphasized to me.
“Are there any other emergency medical conditions — heart attacks, sepsis, broken bones, anything else — where we tell people just to wait until there’s a bed somewhere?” he asked. “For days, a week or two weeks, or months? It’s extremely backwards, extremely unfair to people with psychiatric conditions. And is potentially very harmful.”

Three years after Andy’s death, Louise is focused on raising their daughter, who is now 11 — “our best creative collaboration,” as she put it. Louise teared up several times as we spoke, and said it is still difficult to think about everything Andy went through. She also wonders how hard it must be for people in different circumstances.
“This story played out in the context of someone who had the incredible support of extensive family and friends … who had insurance and a network of people who were trying to advocate on his behalf,” Louise said. “There are people who don’t have that.”
Lainie said she is doing her part to change that in her corner of the world. She has set up a scholarship in Andy’s name for college students studying theater. Last year she got an inquiry about whether students could use the money to cover mental health expenses. Yes, she said, thinking nothing could honor Andy better.
David and a friend started a podcast about mental health. On the podcast, and in a memoir he finished just after their father died last year, David talks about his relationship with Andy and his conviction that psychiatry has become too reliant upon large doses of medication.
Emily, for her part, recently got accepted into a doctoral program in education leadership and policy. Her application essay was about coping with trauma.

On the day that we met outside Emily’s house, she and the rest of her family noted that a difficult and important time of year was approaching. The anniversary of Andy’s disappearance, his birthday and Father’s Day all come in rapid succession starting in late May. Not long after that comes the anniversary of the day police reported the discovery of Andy’s body, which is also the date that appears on his death certificate.
Most likely Andy died well before then. The medical examiner didn’t or couldn’t make a determination and simply needed something for official records. Even so, Andy’s loved ones told me they’ll mark the day as they have every year since, by keeping the Jewish custom of lighting a “yahrzeit” candle.
A properly crafted yahrzeit will burn itself out in 24 hours. Letting that happen, rather than putting the candle out at night, is an important part of the ritual. Its purpose, some rabbis teach, is not so much to mourn as it is to remember the life of the person who is gone and to recognize that the memory of them still affects the living.
That is certainly true for Andy and could someday be even more true if stories like his lead to broader changes in mental health care. Such a shift would improve everyday existence for millions of Americans — and in cases like Andy’s, just maybe, save their lives from being extinguished too early.
If you or someone you know needs help, call or text 988 or chat 988lifeline.org for mental health support. Additionally, you can find local mental health and crisis resources at dontcallthepolice.com. Outside of the U.S., please visit the International Association for Suicide Prevention.

