City councillor doesn't want high-profile incidents to tarnish entire long-term care system
The councillor in charge of Ottawa's city-run long-term care facilities says she's sorry about an incident that left a paralyzed dementia patient lying injured on the floor, but that she doesn't want a few negative high-profile cases to leave people thinking the city's homes are unsafe.
The December 2016 incident involving François Bisson — who died in May 2017 — was one of several that spurred Ontario's Ministry of Health and Long-Term Care to issue a blanket order to the City of Ottawa, demanding it come up with plans to improve the way it runs its care homes.
The order requires the city to come up with a plan to improve the safety and care of patients in its long-term care facilities. It was issued in July, following several investigations into neglect and abuse since 2015 at three of the city's four homes, and was necessary given "the scope and severity of the non-compliances identified in inspections."
The city runs the Peter D. Clark Centre, Centre d'Accueil Champlain, the Garry J. Armstrong Home and Carleton Lodge. Of the four facilities, only Carleton Lodge has not been hit with non-compliance orders in the past three years, according to the order.
The Bisson incident and another high-profile case — that of an elderly resident with dementia being repeatedly struck by a personal support worker — both happened at the Garry J. Armstrong home.
'Very troubling'
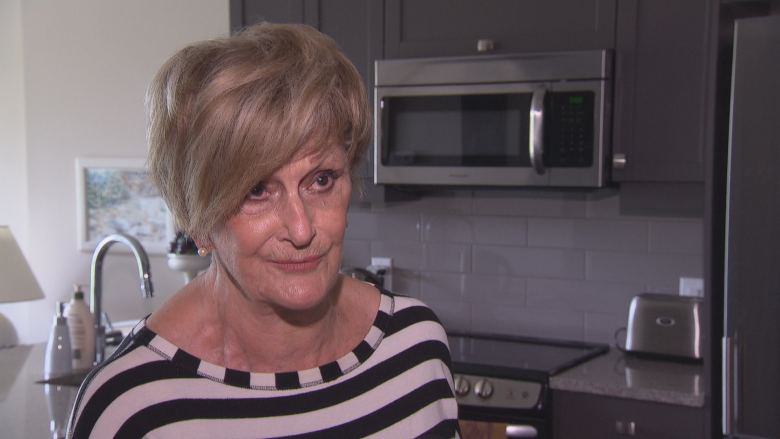
"I'm very sorry that that happened to [Bisson] and to [his wife], because that's very troubling," Coun. Diane Deans told CBC Radio's Ottawa Morning Thursday.
"In that case apparently the resident wasn't properly strapped in — I think it was momentary. But the other part ... is that the employee failed to do the proper reporting, and so that sort of set off a series of events where [Bisson's wife] didn't know what happened.
"That is very troubling to us. That should never have happened. Steps have been put in place to try to ensure that it won't happen again. But it does speak to staff training and the protocols that we have in place."
The city has never been issued this kind of non-compliance order before, Deans said, adding that a number of steps have been taken so far:
- An advisory group has been established that includes long-term care staff, as well as friends and relatives of patients. Its first meeting was scheduled for Thursday, Deans said.
- Working groups are being launched at each of the four long-term care homes mentioned in the order, and will include front-line staff.
- Town halls are being held at the four homes to hear concerns from residents, their families and friends.
- A memo to council was issued by Deans and Mayor Jim Watson Wednesday outlining what they're looking for in a report on the issue from city manager Steve Kanellakos that's due before council Sept. 21.
- Individual workers have been disciplined. Deans said she didn't know what form the discipline took.
- Plans to ensure compliance are being drafted.
'I really believe that they are [safe]'
Deans pointed to a peer review performed in September 2016 by Accreditation Canada, an independent non-profit organization that looks into health-care systems, which she said gave the city's long-term care facilities an overall satisfaction rating of 95 per cent, as well as a 95 per cent compliance rate.
"So I don't want the listeners to think that because there obviously have been some high-profile and very troubling cases, that our homes should have a black eye or are not a safe place for their loved ones, because I really believe that they are," Deans said Thursday.
"But because there have been some high-profile incidents, we obviously at the city are taking this extremely seriously and we have put a whole series of mechanisms in place to try and improve upon what's happening in our homes and to ensure incidents like [this] will never happen again.
"I'm not diminishing that this is very concerning, but also, we're serving 791 very vulnerable residents with 24-hour care, and our average is three hours and 15 minutes per resident of individual care," Deans added.
"I don't want a few cases — that were very troubling and things went wrong, that we have to deal with and take seriously — I don't want [them] to leave the impression with the public that this is systemic in our homes."
Listen to the entire interview with Deans here.
Provincial inquiry
Deans also hopes a provincial inquiry spurred by the Elizabeth Wettlaufer case examines systemic issues in long-term care.
"Based on the level of care that our aging population now needs, based on the complexity of their issues … on the number of cognitive issues, do we still have the right training in place, do we still have the right staff ratios, do we still have the right expertise in those homes," Deans said.
"I trust that the justice … will make recommendations to the province of what they might do in terms of funding and training to ensure that we are providing the best possible care to our vulnerable citizens."