Health-care system is 'broken,' Niagara woman says, after dad suddenly dies in emergency room
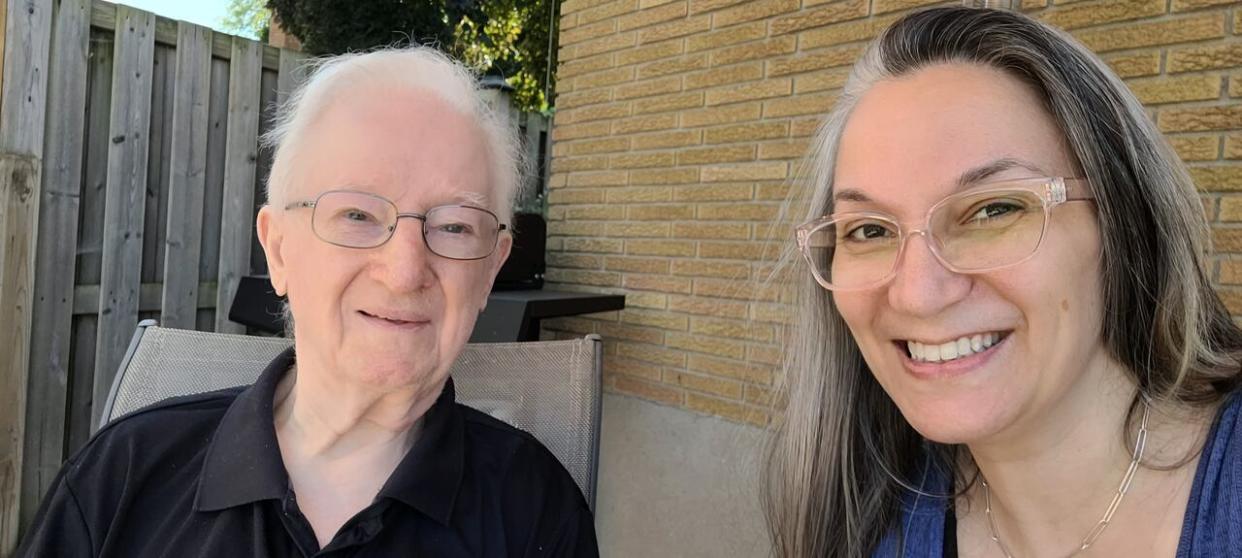
As her father laid sick on on a gurney in a Niagara-area emergency room, Ann-Marie Zammit reassured him he'd recover.
The medical staff at the Welland, Ont., hospital had told her despite an infection, and being in the emergency department for days, CJohn didn't have a fever, his vitals were stable and they'd be conducting more tests the next morning, Zammit told CBC Hamilton in an interview.
She had reason to be hopeful. Before his illness, CJohn, 88, lived independently and was his happy, healthy and quirky self, she said.
But that night at the hospital, CJohn insisted he wasn't going to survive the night.
"He told me his final wishes and I'm like, 'Dad, we're not going to need this because you are going to pull through,'" said Zammit.
The next morning, June 1, Zammit got a call from the hospital. Her dad had died.
"And it was unbelievable because they'd kept telling me that his vitals are stable, his vitals are stable," she said. "Then I got a call from the doctor and he said this was very surprising news."
Zammit doesn't know what caused her father's death, but pointed to the lack of resources at the hospital as significant factors. For example, he'd stayed in the emergency department for several days because there weren't any beds available in other departments to move him to.
"This broken system killed my father," she said.
Hearings taking place across Ontario
Zammit shared her experience at a public hearing in Welland last weekend organized by the Ontario Health Coalition.
The coalition, which advocates for improvements to the public health care system, is documenting experiences like Zammit's at hearings around rural Ontario this month. With input from opposition critics, the network of over 400 grassroot organizations wants to draft recommendations on how to improve local hospitals, especially in rural areas.
The group hopes to provide those recommendations to the province in a report later this fall.

Natalie Mehra, Executive Director Ontario Health Coalition (OHC), is pictured here at a rally in 2019. Mehra says OHC is pushing the Ford government to better fund local hospitals in rural areas with a report it plans to publish in the fall. (CBC)
Executive director Natalie Mehra said it will follow their report last year, which recorded almost 1,200 emergency room closures in the province.
"The goal is to push the Ford government and stop them from continuing to shut down and dismantle public health services and sort of destroy them through privatization," said Mehra.
The province says it's looking at all options to resource hospitals around Ontario.
In an emailed statement this week, Hannah Jensen, a spokesperson for Health Minister Sylvia Jones, said Ontario "is taking bold action to connect more people to the care they need, when they need it."
The province is budgeted to spend $85 billion on health care this year, she noted.
Zammit said she didn't see that funding reflected on the ground.
Staff at Welland Hospital seemed stretched thin, she said, and different doctors came to see him, providing different "patchwork" diagnoses.
CJohn, a diabetic, could barely eat when he was admitted to hospital. Still, it took two days for the hospital to provide him with liquid food, Zammit said, and only after she'd pushed for it.
While CJohn was wheeled into a small room, the emergency department's hallways were filled with patients on gurneys, Zammit said.
"I felt like we were in some sort of field hospital in the middle of the war," she said. "They have no ability to call for the nurse. They just have to yell."
Niagara Health facing staff shortage
In an email, spokesperson Erica Bajer said Niagara Health is unable to confirm or comment on individual cases due to privacy legislation.
Niagara Health is facing a higher volume of patients at emergency departments and a shortage of health human resources, particularly emergency-trained medical professionals, she said.
"We have taken a number of steps to help mitigate this, and continue to actively recruit for both staff and physicians," she said.
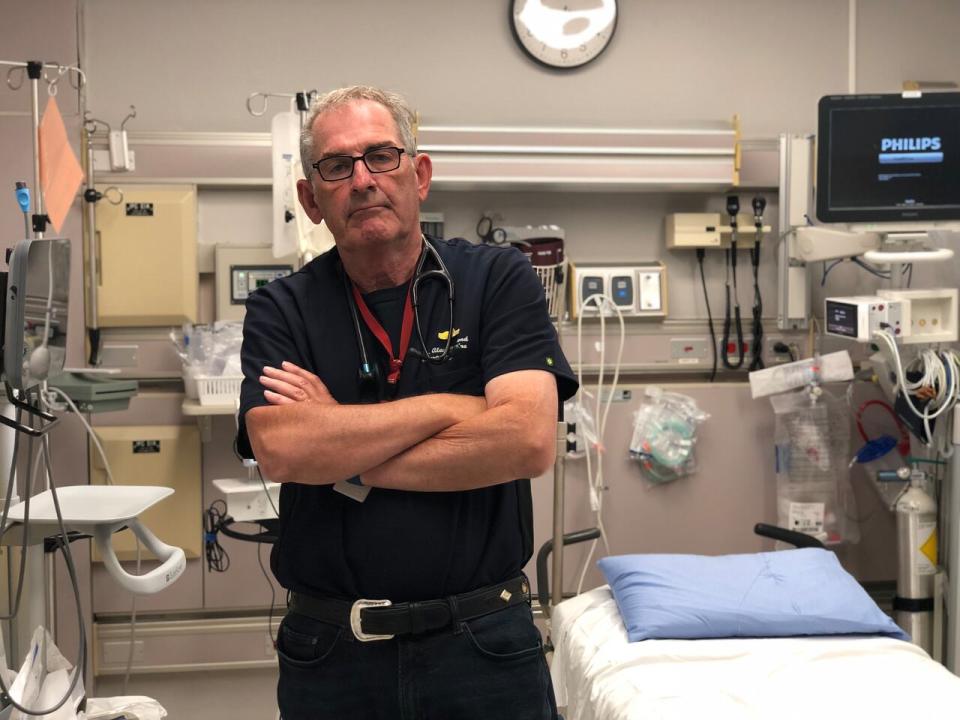
Dr. Alan Drummond, an emergency room physician in Perth, Ont., says hospital doctors and staff are becoming more concerned they're unable to fulfill their mandate due to a lack of staff and resources. (Provided by Alan Drummond)
The people working the front-lines of Ontario's local hospitals are also growing increasingly concerned.
Dr. Alan Drummond, an emergency physician in Perth, south of Ottawa, says the public is losing confidence in health care, and a lack of support has his colleagues starting to feel the same way.
"It leaves emergency health-care providers feeling extremely uneasy, in that we are unable to fulfill our mandate," he said in an interview.
The Ontario Health Coalition is set to release its new report this fall.


