Rural doctors worry proposed changes could lead to 'brain drain'
In the southeast corner of Saskatchewan is a town called Wawota. The town, known for its colourful collection of fire hydrants painted to resemble cartoon characters like Garfield, is home to nearly 550 residents, according to the 2011 census.
"It's a good community and good people around here. Everyone helps one another out," said 84-year-old Clarence Lamontagne, a resident of the town and a former building contractor.
But one of the struggles of rural life — in this, and in multiple other communities across the prairies — is limited access to health care.
Wawota has a local medical clinic, but physicians from Arcola, Sask., are only on site on Mondays and Fridays, and see patients by appointment only.
"These doctors come in two days a week and they're gone. So if you're sick at night, you can't go to your health clinic," Lamontagne said. "You must go 30 miles away."

It wasn't always so challenging in Wawota. In the early 1990s, Wawota had its own hospital with doctors who lived and worked in the community.
"When we got all these cuts, our town was going lower and lower," Lamontagne said. "Of course, when you lose a hospital, then you also lose your drug store, and you lose this and that.
"Then people start going to bigger communities for health reasons. It hurts your area."
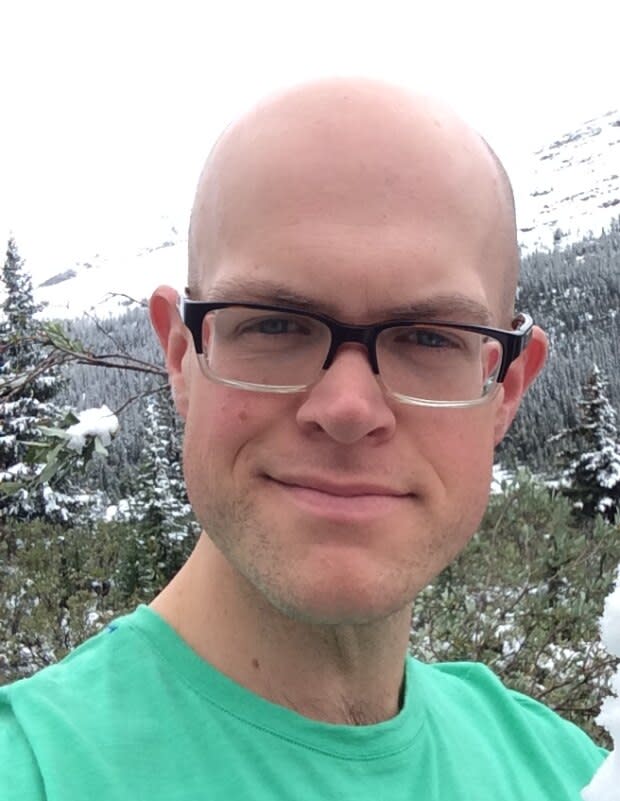
Doctor Matthew McIsaac, who has practiced in various rural communities across Alberta and currently works out of Banff and Canmore, was born in Wawota.
He said cuts to rural health implemented by Janice MacKinnon in 1993, then Saskatchewan's finance minister for the NDP government, led to a "brain drain" in Wawota.
"It killed rural areas, including [Wawota]. We had lost our [family] practitioner to illness. His replacements came and did not stick around due to the pay cuts," he said. "They couldn't find anybody to provide any long-term coverage, and eventually we lost our hospital."
Since that time, McIsaac said the population of the town has dwindled by about 200 people.
"There is evidence, historically, that things like this kill small-town medicine," he said.
This year, MacKinnon was tapped by the Alberta government to lead a six-person panel evaluating the province's finances. In the report emerging from that panel, various recommendations were made to help Alberta to balance its budget, including proposing pay cuts for physicians.
A move to Alberta
Eventually, McIsaac also left Wawota, but kept working in rural communities throughout rural Alberta, including in Coronation, Beaverlodge and Milk River.
Due to higher funding, McIsaac said his time practicing in Alberta was always more fulfilling compared to working in Saskatchewan, as he could take time to help a patient fully and provide complete care.
There are challenges associated with being a rural doctor, McIsaac said — it can be lonely and it can be high-pressure, given the responsibility laid on a limited number of physicians.

So when McIsaac heard about changes proposed by the Alberta government — that would affect how doctors schedule, bill, and interact with their patients, he said it "blew [his] mind."
"It seems like the government is completely non-thinking and quite hubristic with their approach here, in believing that they've found an answer," McIsaac said. "Or, there's this cynical view that they actually want to sacrifice rural care."
Changes proposed by the Alberta government were communicated to the Alberta Medical Association (AMA) on Nov. 14. Rural doctors say those changes, among others, would disproportionately affect their practices.
Earlier this year, Alberta Health Services reduced the amount it pays doctors to be on call after funding was reduced to its specialist-on-call program by $10 million per year.
"They cut that without warning quite recently and already the family physicians were quite up in arms, because that's a big part of their livelihood," McIsaac said. "But the second thing that's come now is this proposal that the complex modifier fees get cut."
Under the proposals, doctors would be paid the same for a 25-minute visit as they are for a 15-minute visit, and funding would be cut for complex care plans.
"These physicians working in rural centres are looking to face between, at the low end, a 10 per cent cut up to a 40 per cent cut for some of them in their billing, almost immediately, because of this," McIsaac said. "So you've just been cut in terms of your night call, and now you'll see [complex modifier fees cut]. Then, you're suddenly on par with places like British Columbia, or Ontario, or Saskatchewan, which is the goal of the government.
"Well, to live in a place that is remote and rural, or to move to a place like Penticton or Kelowna or Victoria seems like a no-brainer when the pay is equal and when the cost of living is not much different."
Some say advanced skills also threatened
Michael Beach is a family physician with training in anesthesia who practices in Drumheller, Alta., and said those working in rural settings with advanced skills would be "very disproportionately impacted" by the changes.
"It impacts us the same way as a lot of the urban doctors, but there are a few things that impact us even more so and threaten those advanced skills in the rural setting," Beach said.
The reduction of call stipends would make a big impact, Beach said, calling them a "huge incentive" to work in rural Alberta.
Steve Buick, a spokesperson for Health Minister Tyler Shandro, wrote in a statement that those incentives were left over from former regions that competed for doctors by paying them extra.
"A decade ago we had an overall shortage, today we don't," he wrote. "We don't need to pay much higher rates than other provinces when we don't have a shortage anymore. We can make some modest reductions."

But Beach said that while he understood what's being argued — that doctors are working full-time during their call shift, and should not get a stipend on top of being paid continually — he said that only applies in urban settings.
"That's not true in the rural setting at all. When we're on these call shifts, we're not continually providing fee for service work throughout," he said. "For the duration of time this whole week that I've been on my call shift, I can't leave Drumheller, I can't go for a walk with my wife that's a half-hour away from my home and my car, because I could get called at any moment to go do [anesthesia]."
Right now, we're going to wait and see, but our minds are very open to leaving [Alberta]. - Michael Beach, Drumheller family physician
Plus, according to Beach, the whole reason doctors take positions in rural Alberta is because of call stipends.
"If you lose those, in my opinion you're going to lose a lot of people who say, 'It's just no longer worth the effect on my personal life and family life and lifestyle to continue to provide this service for no compensation whatsoever,'" he said. "You're looking at a potentially large reduction in some of those services in a lot of these smaller centres."
The spending question
Alberta today spends the second-most on healthcare, behind only Newfoundland. In his statement, Buick said government would listen to proposals offered by the AMA related to getting costs in line to other provinces.
"Some people are overreacting to our proposals and saying doctors won't be able to do good primary care. The proposals are common sense and aligned with other provinces," Buick wrote. "They don't limit physicians' ability to provide high-quality care, they just reduce the excess amounts we've been paying."
The proposals are common sense and aligned with other provinces. - Steve Buick, spokesperson for Health Minister Tyler Shandro, in a statement
In a joint statement attributed to AMA president Christine Molnar and AMA rural medicine president Edward Aasman, cuts proposed by government to rural medicine could be "immense."
"The effect would be absolutely devastating on those practices," the statement reads. "Rural practices are already struggling to remain stable, including attracting and retaining physicians. If implemented, these proposals could severely threaten the viability of those practices."
With all the proposed changes considered, Beach estimated he would be looking at at least a 30 per cent reduction in his salary.
"My wife and I have actually sat down and looked at it and said, 'If all of these things come to fruition, would we stay in Alberta?'" Beach said. "Right now, we're going to wait and see, but our minds are very open to leaving if [these changes go through]."
Addressing potential rural shortages
Even if AMA negotiations don't go as planned, the Alberta government may have a card up its sleeve to address any shortage of rural doctors that would result from funding changes.
Bill 21, otherwise known as the Ensuring Fiscal Sustainability Act, allows the province to tell new doctors where they must practise medicine in Alberta, based on the recommendations of an expert panel.
Beach said he found that move counterintuitive, given the possible impact of changes being proposed.
"The reason why a lot of things were put in place over the last 20, 30 years, is because we had such a shortage of rural doctors. We had to find ways to incentivize people to come," he said. "That started to work, and now we're taking steps back. Forcing peoples' hands on where they're going to go simply isn't going to work.
"All that's going to happen is, trainees will just finish off their medical education and say, 'if I don't want to work in rural Alberta, I'll just go to another province.'"
The AMA is currently developing its response to the proposed changes, and plans to submit its feedback prior to the Dec. 20 deadline.


