Scientists think nightmares and hallucinations could be an early sign of autoimmune diseases
A recent study identified unusual symptoms that could indicate the flare-up of some systemic autoimmune rheumatic diseases.
Nightmares and "daymares" - hallucinations experienced while awake - have been shown to be potential warning signs of the onset of some autoimmune diseases such as lupus and rheumatoid arthritis.
"One interesting finding was that certain symptoms, including nightmares, were commonly described as happening just before the other disease symptoms, and so may provide an early warning system of increasing disease activity. This could lead to earlier treatment and better support," said Melanie Sloan, the lead author and a researcher in the Department of Public Health and Primary Care at the University of Cambridge.
According to Sloan, the team was able to get these results by adopting a patient-focused approach, emphasising the patients' experiences and their descriptions of symptoms, rather than relying solely on the observations of doctors and researchers.
"Some of the symptoms we asked about were commonly known to be a part of lupus (for example headaches and fatigue); other symptoms were not currently listed under any criteria for lupus or other systemic autoimmune rheumatic diseases. This included nightmares," Sloan said.
The study was published this week in the journal eClinicalMedicine.
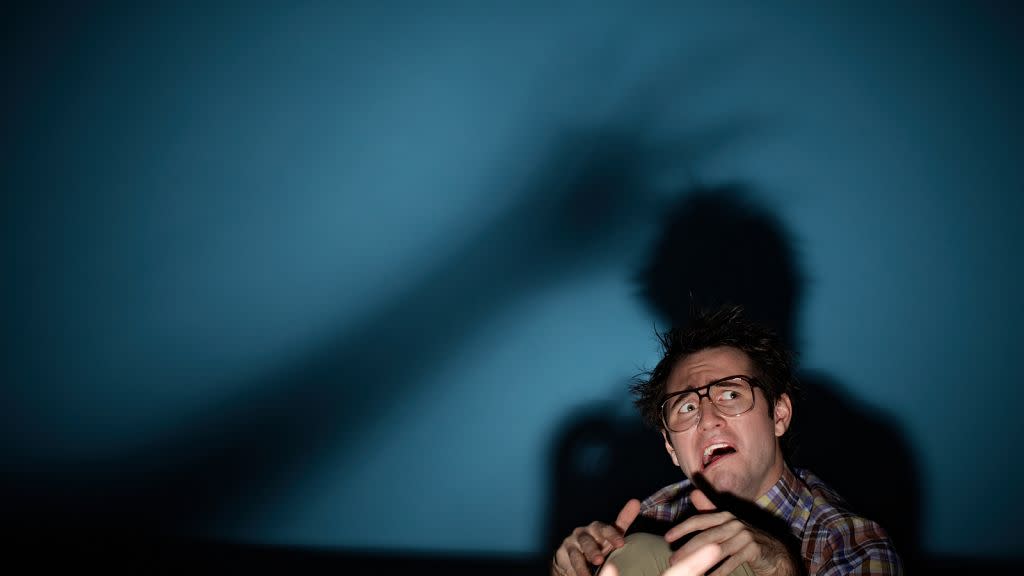
Nightmares featuring violent themes
The nightmares and hallucinations experienced by patients, as reported in the research, often feature recurring frightening and violent themes
For example, one patient from Canada described them as "usually quite frightening, like there’s a serial killer after me, and the last few years, I have the same one".
"He’s got my legs or something, I can still feel something on my legs even when I’m then awake," the patient added.
Another patient from England described a recurrence of nightmares in which they are the perpetrator.
"I have lots of violent dreams… one of them was somebody attacking me and I ended up slitting their throat. Oh I mean, really nasty. I mean I'm not a violent person at all. I don't even kill an insect," the patient said.
While many patients are reported to have experienced nightmares and “daymares” to some degree, it remains unclear whether these neuropsychiatric symptoms could serve as a reliable indicator in undiagnosed cases.
"It is difficult to tell which symptoms preceded diagnosis as a major limitation of our study was that we were relying on people remembering when their symptoms first happened and some were many years ago," Sloan said.
"Many people had also not thought about nightmares possibly being related to their disease before".
Neuropsychiatric symptoms
Some symptoms that commonly occur at the start of flares include increased fatigue, sensory symptoms (such as tingling in the hands), cognitive problems, and mood changes.
However, according to Sloan, the study found that although the symptoms leading up to a flare-up are consistent, they tend to vary among patients.
While one patient might experience cognitive issues, loss of balance, and heightened anxiety before a flare, another could suffer from nightmares and a "feeling of unreality," making it challenging to establish a standard list of symptoms to monitor.
For example, lupus, a long-term autoimmune disease where the body's immune system mistakenly attacks its own healthy tissues, is characterised by its heterogeneity, presenting with over 100 possible symptoms across the body, according to Sloan.
In this case, while impacts on the kidney can be detected through urine tests and kidney biopsies, and skin or joint involvement may be visible to the clinician, Sloan emphasises that most symptoms are neither visible nor detectable in tests.
"This is particularly the case with the neuropsychiatric symptoms, which are reliant on good patient-clinician communication to detect," Sloan told Euronews Next in an email.
'Journey to diagnosis can be long and traumatic'
Sloan adds that many patients have reported that their neuropsychiatric symptoms were not taken into consideration as warning signs of an impending flare-up.
Patients often say their symptoms are "not understood, dismissed as not part of the disease, or even disbelieved by their doctors," making it difficult to recognise an approaching flare and to implement a treatment plan to mitigate its severity.
"Unfortunately, as we are about to report in our next study, the journey to diagnosis can be long and traumatic, and have a persisting and devastating impact on people's self-esteem and trust in doctors," Sloan said.
She emphasises the importance of doctors listening to patients and valuing their perspectives, especially regarding neuropsychiatric symptoms, which are largely subjective and not visible.
"They are the ones living in the bodies experiencing these symptoms after all, and so ideally placed to monitor the changes as a flare is about to start," Sloan said.


