UK E. coli outbreak: What are the symptoms and how does it spread?
Stomach bugs are always unpleasant, leading to days of tummy problems that can leave you housebound. While the cause is rarely clear, thousands of cases in the UK every year are a result of eating food that has been contaminated with E. coli.
It’s impossible to completely eliminate the risk of coming into contact with harmful strains of the bacteria, but you can arm yourself with the knowledge of which symptoms to be wary of and tips on how to reduce your chance of becoming infected. Read on for the best way to protect yourself.
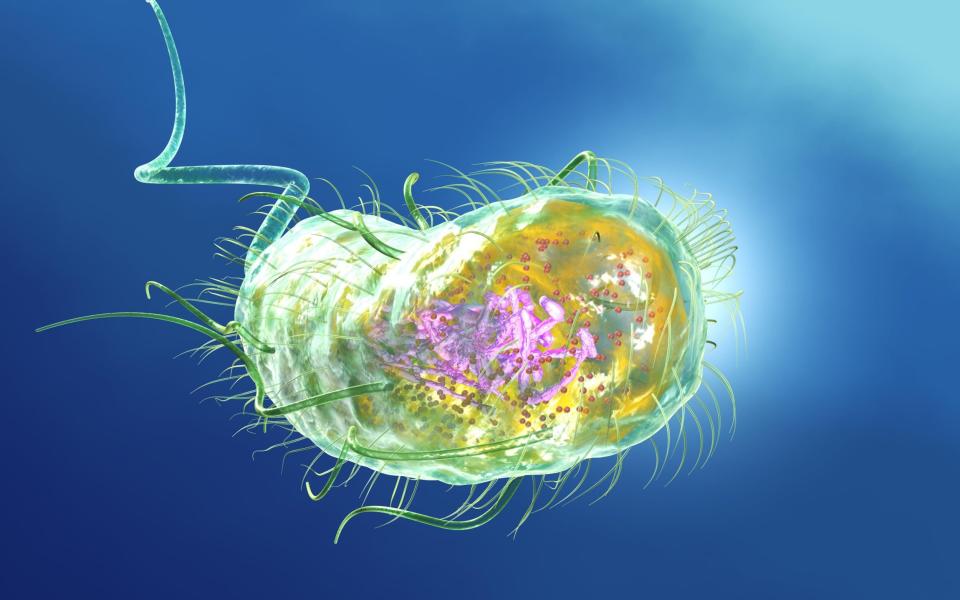
What is E. coli?
Escherichia coli (E. coli) bacteria is commonly found in the gut of people and animals and is excreted from the body in faeces.
Most E. coli strains are harmless and the majority of those living in our gut are even beneficial, as they aid digestion, says Dr Alex McCarthy, a senior lecturer in the Department of Infectious Disease at Imperial College London. “However, some E. coli can cause illness.”
The vast majority of intestinal E. coli infections in the UK are caused by Shiga toxin-producing E. coli (STEC) O157, says Alan McNally, a professor of microbial evolutionary genomics at the University of Birmingham.
An outbreak in the UK this month was caused by the STEC O145 strain. “It’s a bit of a new kid on the block,” says McNally. “O145 is not particularly common, which is what allowed the UK Health Security Agency (UKHSA) to identify that it was probably an outbreak.”
STEC strains are a health concern because they produce toxins called Shiga that can damage cells in the intestine, which stops it from working as it should, says McCarthy.
Symptoms of an E. coli infection and how long it lasts
Stomach cramps
Diarrhoea, which is often bloody
Nausea and vomiting
Typical symptoms of a STEC infection are diarrhoea, stomach cramps and vomiting, which usually occur within three to four days of being exposed to the bacteria.
“Within a short space of time, you will start to see blood in the diarrhoea – that’s usually a pretty good indicator that you’ve got a STEC infection,” says McNally.
Can E. coli kill you?
In severe cases, a STEC infection can lead to blood clots that can be fatal. “This happens when blood vessels in the intestine that have been damaged by Shiga toxins form blood clots that travel through the body,” says McCarthy.
If the toxins reach the kidney, it can lead to a condition called hemolytic uremic syndrome (HUS) and kidney failure, which can be fatal, he explains.
“The vast majority of people that get [STEC] will not suffer that severity of infection, but it can happen,” notes McNally.
Young children, the elderly and immunocompromised are most at risk. In these cases, their health would deteriorate quickly and they may complain of:
Back pain
Have blood in their urine
Have a severe fever
“At that stage, don’t mess around – call 999 or go straight to A&E,” says McNally.
Where is E. coli found?
Food which comes into contact with manure
Petting farms
Contaminated water
STEC is regularly found in the lower intestine of animals, especially cows, but also sheep and goats, and doesn’t cause them any problems, says McNally.
However, if manure from these animals infiltrates food, it can cause infections in people.
This contamination can occur due to food, such as meat or dairy products, coming into direct contact with animal faeces during the slaughter process. If this meat is then raw or undercooked when people eat it, they are likely to become unwell, says McCarthy.
Alternatively, if manure gets into the water supplies for farms, which is then used to water leafy greens and vegetables, people can become infected, he explains.
When STEC O157 was identified in the late 1990s at a butcher’s shop in Wishaw, Scotland – in one of the world’s worst outbreaks to date – it was associated with poor hygiene from handling raw food, says McNally.
“Then we got a lot of cases from petting farms, which is why they are now quite strict with hygiene measures there,” he says.
“Now what we’re seeing more and more is outbreaks associated with pre-packed salads and processed foods – basically anything where the food isn’t cooked but is pre-packed, processed and nationally distributed.”
For example, an outbreak in Germany in 2011, that infected thousands and killed dozens, was traced back to bean sprouts. “Outbreaks tend to be big because it’s very difficult to identify the foodstuff that’s been contaminated,” says McNally.
Drinking contaminated water from lakes, rivers or taps can also cause a STEC infection, says McCarthy. Swimming in pools or the sea can also pose an infection risk but this is less common, he says. “To minimise the risk, it is important that you do not swim in dirty water or swallow the water,” he adds.
Is E. coli contagious? How does it spread?
When it comes to transmission, “people shouldn’t fear that they’re going to get this from the person sitting next to them – it’s not like Covid, that’s not how they spread,” says McNally.
However, it can spread between people through the faecal-oral route of transmission. This occurs if an infected person does not correctly wash their hands after using the lavatory and handles another person’s food.
The UKHSA warns that the bacteria can spread within families and in nurseries, schools, care homes and hospitals.
How can you prevent it?
Regularly wash your hands with warm water and soap (alcohol gels do not kill all bugs)
Wash fruit and vegetables and cook food properly
Do not prepare food for others if suffering from diarrhoea and vomiting
Don’t return to work, school or nursery until 48 hours after symptoms have stopped
Use disinfectants to clean surfaces
Tens of thousands of foods vulnerable to E. coli contamination are distributed across the country every week and only a handful of people become unwell, so a person would be unlucky to become infected, says McNally.
However, there are some steps people can take to reduce their risk of consuming the bacteria.
“In our house, we always wash every bit of fruit and veg before it’s consumed,” says McNally. “If you’re buying a pre-packed salad from a shop, there’s a benefit to washing it.”
He also recommends being “very cautious” about consuming unpasteurised dairy products and raw milk (which haven’t been treated to kill harmful bacteria). “There is always the possibility of some faecal contamination of those dairy products as they’re made.”
How can you treat it?
“If you see blood in your stool, then you should be contacting the doctor because it’s important that as many cases as possible are notified to the UKHSA,” says McNally.
However, while diarrhoea is unpleasant, it is self-limiting, so should pass on its own without treatment, he says.
There is no specific treatment for a STEC infection but it’s important to drink plenty of fluids as diarrhoea can lead to dehydration, says the UKHSA. The NHS advises drinking small sips of water often and eating solid foods as soon as you feel able to, while pharmacists may also recommend using rehydration powders.
If a STEC infection lasts for more than a week, then go back to the doctor. “Treatment options are tricky because STEC produces toxins when they come under stress, such as when exposed to antibiotics,” McNally says.
As a result, doctors don’t typically prescribe antibiotics and would favour letting the illness run its course, unless it is a very serious case.


