Why err on the side of caution as COVID-19 looms in health-care workplaces

Hospitals, long-term care homes and other workplaces in Canada need to err on the side of caution or risk being paralyzed in the face of uncertainty from COVID-19, some doctors say.
Six months after the country's first presumed case, more than 8,900 devastating deaths have occurred mainly among elders and 98,000 others have recovered. Restrictions to everyday routines curbed transmission and avoided overwhelming health-care systems, but public health officials warn people still need to protect themselves to keep case numbers low.
COVID-19 is a tricky disease. Its symptoms can be absent or vague, its course remains unpredictable to physicians and its exact methods and timing of transmission haven't been nailed down.
Those lingering uncertainties are on Dr. Lauren Crosby's mind as Calgary ramps up day and elective surgeries.
"When you're working in the context of scientific uncertainty, especially in the case of an impending and serious threat to health, it's unreasonable to clarify, to wait for the answers to all your questions before you take action to avert the threat," said Crosby, an anesthesia resident in Calgary.
Reassurance of higher-level precautions
That's why Crosby and her father, Dr. Edward Crosby, an anesthesiologist at Ottawa Hospital, wrote an opinion piece last week in the Canadian Journal of Anesthesiology titled "Applying the precautionary principle to personal protective equipment (PPE) guidance during the COVID-19 pandemic: did we learn the lessons of SARS?"
"If we can't be certain then we should be safe," she said.
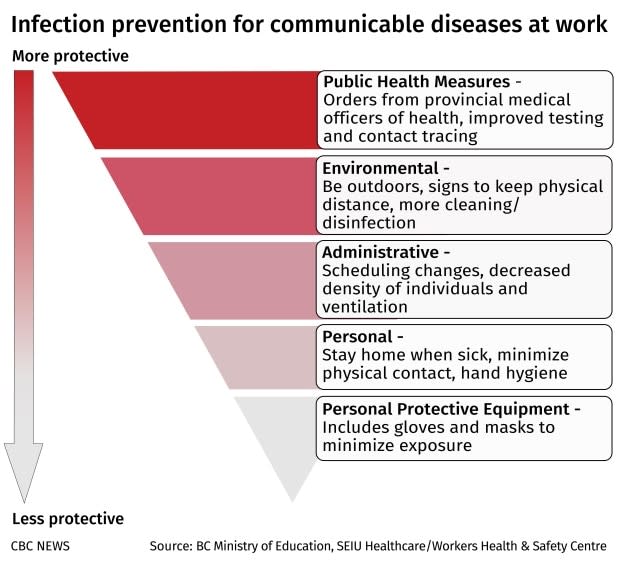
For the Crosbys, one of the lessons from the 44 deaths from SARS in Toronto in 2003 is that when health-care workers are asked to put themselves at risk of infection to care for others, PPE like masks, gowns and gloves should be provided. It's an application of the precautionary principle — the idea of erring on the side of caution to protect public health.
Justice Horace Krever first recommended the precautionary principle during the Commission of Inquiry on the Blood System in Canada in 1997.
Justice Archie Campbell's 2006 SARS Commission also called for the health concerns of health-care workers to be taken seriously so they feel safe, even if that requires higher levels of precautions, Crosby said.

If health-care workers become sick with COVID-19, they pose a "triple threat" as vectors for more disease transmission, reduced capacity in the health-care system and by becoming patients.
"Scarcity is not a valid reason to limit protective equipment and to limit access to that equipment," Crosby said.
Instead, she said, to prepare for a second wave, PPE should be used as efficiently as possible, including decontaminating and repurposing it and using other barriers during procedures that spray infectious aerosols.
Fostering public trust
People working in any industry need to feel involved in decision making and have their concerns addressed, Crosby said. Otherwise, there can be a loss of public trust, low morale, anxiety and confusion. In health-care settings, the stress can lead to burnout of workers who are particularly in demand during the pandemic.
WATCH | Lives remembered in Quebec:
Dr. Roger Wong, a clinical professor of geriatric medicine at the University of British Columbia, called the idea of applying the precautionary principle an important and timely conversation because COVID-19 has already hit long-term care homes and other shared living facilities hard.
"We have an opportunity, a very narrow window," Wong said in an interview. "We should take action now."
How? Wong told a Senate committee reviewing the government's response to COVID-19 that he'd like to see systemic changes, such as including long-term care within the Canada Health Act.
The federal government is well positioned to set standards in areas like collecting physical and mental health outcome data, including social isolation and loneliness. Then, the data can drive policy change and better protect those who are most vulnerable, Wong said.
Wong was also involved in updating the federal government's COVID-19 guidance for long-term care homes.
Be transparent as evidence evolves
Tim Caulfield, Canada research chair in health law and policy, supports applying the precautionary principle.
He said it has an intuitive appeal. During COVID-19, it's been raised in the context of wearing masks and weighing the use of pharmaceutical treatments like hydroxychloroquine.
"If you're going to do that, then you have to take extra care to ensure that you're being transparent about the information that you're using, the evidence you're using to make the decision," Caulfield said. "You want to make sure that you are open to change as the evidence evolves."
He pointed to an association between jurisdictions around the world, such as Australia and regions of France, which have been the most successful in containing the disease so far, and public trust in key institutions and decision makers.
"In the face of uncertainty, we still have to march forward and we have to do it in a manner that benefits the most, and I think that we can't allow uncertainty to paralyze us," Caulfield said.
Dr. Timothy Paul Hanna, a clinician and scientist at Queen's University Cancer Research Institute, applied the precautionary principle to help guide Ontario's prioritization plans for cancer care during COVID-19.
Potential risks to patients include:
Infection risk by leaving their homes to come for treatment.
Possible side-effects of treatment, such as radiation for lung cancer that further diminishes lung function after getting COVID-19.
Treatment and diagnostic delays associated with rationing care when hospitals scale back.
"We're really fortunate across Canada," Hanna said. 'We weren't left as single institutions or single physicians to proceed based on our own opinion when resources became limited. I think that that's a real plus of our universal health-care system."
Provincial prioritization frameworks weighed factors he wrote about such as the magnitude of benefit from treatment, if the treatment is meant to be curative or palliative, patient considerations such as age, comorbidity, and preferences as well as the availability of human resources and equipment to treat cancers.

"Regardless of how we discover how well we might have done, I think the mental health effects and social stress, the impacts on patients and their families having to wait or having to experience care in maybe a different way, like through telemedicine or other virtual means, I'm sure we'll find has been hard on patients."
Canadians are touched not only as patients, but as employees and citizens, too.
Soma Ray-Ellis, chair of the employment group at Gardiner Roberts LLP in Toronto, said that as non-essential employees return to work and social gatherings occur, more direction is needed on applying precautionary principles together with human rights, occupational health and safety and privacy legislations.


