B.C. centre planning clinical trials to treat addiction with hallucinogens
British Columbia's fledgling network for research into drug abuse is planning clinical trials to explore treating opioid addiction and other substance abuse disorders with hallucinogens.
The B.C. Centre on Substance Use will examine the effectiveness of psychedelic drugs to help people battling addiction. One of the organization's lead researchers and directors, Dr. Kenneth Tupper, says the trials are set to begin this year, pending procurement of funding.
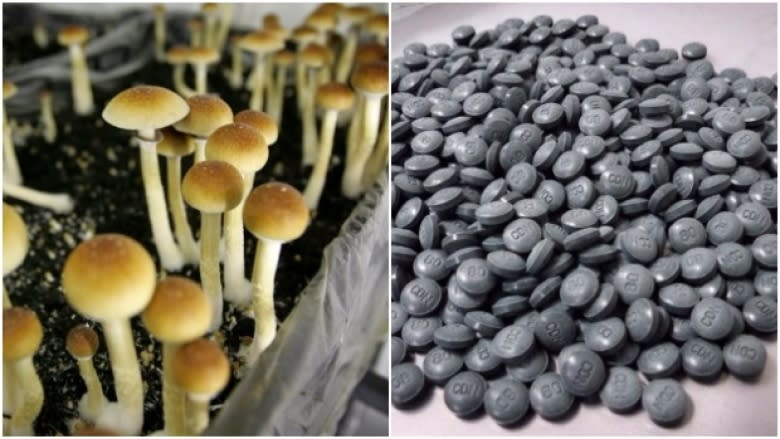
"The evidence from renewed research in this area ... is that there's clinical therapeutic potential for drugs like psilocybin, LSD, [and] ayahuasca," said Tupper, adding B.C. and Canada are lagging behind in the research field.
Tupper says hallucinogens could play a role in the province's growing opioid crisis, which claimed 120 lives in March alone. The BCCSU was established by the provincial government to explore solutions to the health crisis, as well as enhance addictions research in B.C.
Promising research
Psychedelics have long caught the attention of addictions researchers, and numerous clinical trials have shown promising results.
A 2014 study from John Hopkins University, for example, found psilocybin (the active ingredient in magic mushrooms) to be an effective tool to help smokers kick their habit, more than doubling the effectiveness of traditional cessation drugs like varenicline.
"Canada was once a world leader in this area of research back in the early 1950s and 60s — and we're now kind of lagging behind," said Tupper, adding that Canada pioneered the exploration of treating alcoholism with LSD — a treatment mechanism that continues to be studied.
"The BCCSU is well positioned to undertake this kind of research," he said.
How it works
Tupper says each potential patient will undergo a thorough screening process prior to being admitted into the trial. He says patients with mental illnesses such as schizophrenia or bipolar disorder might not be well suited for treatment.
Once admitted, patients have sessions with a team of therapists who talk them through the experience of taking the medication. Tupper says patients typically have one to three monitored therapy sessions where they ingest the hallucinogen.
"It's often very unremarkable in these sessions themselves. People are usually wearing a blindfold, listening to music, and encouraged to introspect and reflect on their lives," said Tupper.
But the "unremarkable" sessions can encourage subjects to make significant life changes, like overcoming their addictions.
"Therapeutic outcomes ae often correlated with a mystical or a spiritual-type experience. People often have deep insights about themselves and their relationships with others and with God — and sometimes, as a consequence, have significant behavioural changes."
Life and death
Tupper says patients follow up with clinicians to determine desired health outcomes, and the team works with the individual to reach those goals.
And with all eyes staring at B.C.'s ongoing opioid crisis, Tupper hopes that assisted psychedelic therapy could become part of the solution.
"It's a matter of life of death," he said. "There's an urgent need to explore all different kinds of options and this is one that seems to be very promising."