Experts weigh in as N.B. changes COVID-19 PCR testing policy to require medical referrals

An Atlantic region scientist who studies immune system responses to viruses says he supports the further cutback in COVID-19 PCR testing, which takes effect in New Brunswick today, while an infection control epidemiologist calls the move "unfortunate" but not surprising.
New Brunswickers who have COVID-19 symptoms can no longer self-refer for a PCR (polymerase chain reaction) test, which is processed in a lab and considered the gold standard for diagnosis.
PCR tests are now only available to people with symptoms for whom "the outcome of PCR testing will directly influence treatment or care" — and they require a referral from a health-care provider, such as a doctor or nurse practitioner.
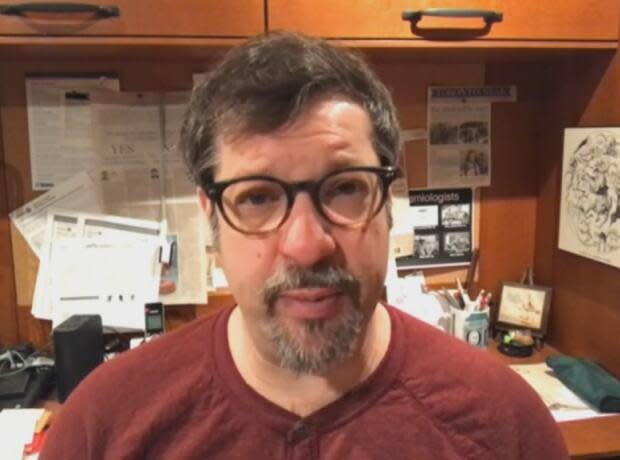
"I'm not sure there are many situations right now where … you would need a PCR test, you know, if you already have access to a rapid test," said Rod Russell, a professor of immunology and virology at Memorial University in Newfoundland and Labrador,
"And that's maybe the key right there, is the access to the rapid test, right?"
Millions of rapid tests in stock, says chief medical officer
Rapid tests, also known as point-of-care testing (POCT) kits, are still available for pick up by appointment in New Brunswick through various community-based sites, such as public libraries, municipal buildings and health centres.
According to the federal government's website, the province only has about 337,000 rapid tests in inventory, as of March 22. That's nearly a 47 per cent drop from a month ago.
But the distribution information provided on the federal government's website represents "an estimated inventory based on their distribution alone," said Department of Health spokesperson Shawn Berry.
"New Brunswick has its own reserve of rapid POCT tests above what is reported on the federal government's website," he said in an email.
The province has millions, according to Dr. Jennifer Russell, the chief medical officer of health.

The federal government stopped shipping rapid tests to provinces and territories at the end of January, but still has about 50 million allocated to them, "which will be held for readiness in case of future need," a Health Canada spokesperson has said.
Colin Furness, an infection control epidemiologist and assistant professor at the University of Toronto, said he understands providing PCR tests has been expensive, and they're so sensitive they can detect a past infection when the person is no longer actually contagious, which is "problematic."
He contends PCR testing was most useful earlier in the pandemic "when we were trying to have no COVID at all.
"Knowing that you had an infection, whether you were infectious or not, was actually really valuable information — for contact tracing, for understanding the behaviour of the virus," he said.
"Those days are long gone."
Savings come at a cost
Furness is firmly opposed, however, to any winding down of rapid tests. Although they're less sensitive than PCR tests, they're arguably "more socially useful."
"They answer actually a far more useful question than, 'Is there COVID in my body?' And that question is, 'Am I infectious right now?'"
Not providing ample supplies throttles "an enormously useful tool to help people take agency and understand what is happening to their bodies and to be able to make smart decisions about other people … in terms of putting them at risk."
While rapid tests also cost a lot cumulatively, so does having people absent from the workforce, and ICU beds and long COVID, he stressed. "There's a cost of doing nothing. There's a cost to letting it run rampant."
'Learning to live with the virus' phase
Russell says people everywhere are testing "less and less."
He suspects other jurisdictions will also soon further restrict PCR testing, if they haven't already.
"I think the 'learning to live with the virus' phase is well upon us."
At this point, many, if not most people have already had COVID and "survived," and aren't worried about getting it again, said Russell.
"There's this feeling that we need to, you know, just move on now. And unfortunately I think a lot of people aren't even bothering to test."

The pandemic is not over, he said. There are still people getting sick and dying.
There are also still people who haven't contracted the virus yet, some of whom are vulnerable and afraid.
Cutting back on PCR testing increases the risk those individuals will get exposed to the virus, said Russell.
Reduced testing also means reduced surveillance, he said.
Although there isn't the same urgency to COVID testing and surveillance as there was during the peaks of some earlier waves, it's important to maintain levels higher than they were pre-pandemic, "so that we don't get caught unaware if it happens again.
"And it could happen again," he said, pointing to the bird flu virus H5N1, which is circulating in parts of Canada and transmitting to other animals.
Could impact surveillance
PCR tests are used to calculate positivity rates, which indicate the level of transmission in the community and level of risk. The province includes this data in the weekly COVIDWatch reports.
If the number of PCR tests being conducted drops a lot with the new referral requirement, the Department of Health may decide there isn't enough data to "provide a meaningful summary," noted Furness.
"That would be a legitimate concern because when too few people are being tested, you actually don't know if the data you're posting are really reflective of what's going on. Your confidence starts to drop."
If testing and surveillance are cut back too much, there is also a risk of missing new variants of concern, said Russell.
"There is a feeling amongst the virology and immunology communities right now that we're probably going too far back," he said.
PCR tests offer a scientific advantage because unlike rapid tests, which people do at home and throw out, the samples are collected and can be stored for later sequencing to check for new variants, Russell said.
But if there are any new variants of concern circulating, people would probably be showing up in hospital, where PCR tests are still being done anyway, he noted.
There are also other ways to monitor, such as wastewater testing, which is currently being done in only Fredericton and Moncton.

Furness contends wastewater testing is the best monitoring tool available because it doesn't rely on people seeking out testing, or self-reporting results, and can serve as an early warning of rising levels, whereas hospitalizations and deaths lag.
People who are infected shed the virus in their feces in the form of a genetic material called ribonucleic acid, or RNA, which can be found in raw sewage, typically five to seven days before they develop symptoms.
Wastewater testing is also "very cheap," according to Furness, and once the infrastructure is in place, can be used to track any future types of outbreaks, he said.
"If I were New Brunswick, I would be spending a small amount of money to do a lot more wastewater testing. A lot more."
Furness also urges officials to move toward measuring population health according to the harms associated with COVID-19. He cites screening for COVID-associated diabetes as an example.
"The sooner that you can catch cases, the sooner they can be managed and the better outcomes you have."


