What to know about Paxlovid, the COVID antiviral that keeps people out of the hospital
The antiviral Paxlovid has changed the battle against COVID-19.
It's so effective that more than 85% of people at risk for severe disease can avoid a bad outcome with a five-day course of the prescription medication given within five days of symptoms starting.
But word of its effectiveness has been slow to catch on. Only about 7.6 million Americans have taken the medication, with nearly 1.6 million doses currently available nationwide.
People have been apparently scared off by misinformation and side effects – one that'sminor and goes away after the medication's five-day course and the other that might not be due to the drug at all.
And doctors, concerned about interactions with other medications, have withheld Paxlovid from vulnerable people rather than stop the other drugs for a handful of days.
This has left only a fraction of those eligible receiving them, despite a strong lobbying effort by the Biden administration and public health officials.
Latest news:
Here's a primer on how the antiviral works, what it does and who should get it.
How does Paxlovid work against COVID-19?
Like other antivirals, Paxlovid is designed to stop a virus from making copies of itself. Limiting the number of copies helps the immune system fight off the virus.
Made by Pfizer, Paxlovid is a combination of two drugs: ritonavir and nirmatrelvir.
Nirmatrelvir, an oval, pink pill, is a so-called protease inhibitor – the same type of drug that turned HIV into a manageable disease. It stops the SARS-CoV-2 virus from replicating.
Ritonavir, a white or off-white pill, boosts the activity of nirmatrelvir.

How long does it take for Paxlovid to kick in?
Paxlovid is given in a five-day course with three pills taken twice a day. Most people report feeling better by the second or third day on the drug.
Pfizer only studied the medication for the full five days, so people should take them as prescribed, said Dr. Aida Habtezion, Pfizer's chief medical officer.
How to get a Paxlovid prescription
Paxlovid is given only by prescription and can be administered by physicians, pharmacists, advanced practice registered nurses, and physician assistants who are licensed or authorized under state law to prescribe antivirals.
The medication is available at pharmacies nationwide, and the government sponsors a "test-to-treat" program in various locations nationwide as identified on this searchable website.
Getting tested quickly after symptoms appear is important because the medication must be given within five days of the first symptoms to be effective, Habtezion said.
Who is eligible to receive Paxlovid?
Anyone aged 12 and older, has symptoms and is at high risk for severe disease is eligible to receive a free course of the medication, funded by the government.
Because so many common conditions, such as obesity, put people at risk for severe disease and because everyone over 50 is eligible regardless of health status, the majority of adults qualify.
Many people are taking it now beyond the narrow restrictions used to initially prove the drug's effectiveness. It's not clear, for instance, whether Paxlovid provides substantial benefit to a young, otherwise healthy adult.
But Dr. Wes Ely, a critical care and pulmonary medicine expert at Vanderbilt University School of Medicine in Nashville, said he doesn't see a reason not to take it. "The potential for benefit is there and the potential for risk is very low."
Potential Paxlovid side effect: Metallic taste in mouth
Paxlovid's primary side effect is a metallic taste in the mouth during the five days of treatment. It goes away at the end.
"The side effect profile, other than the taste, is extremely tolerable," Ely said. "Most people will have no side effects from that drug."
'Rebound' and Paxlovid
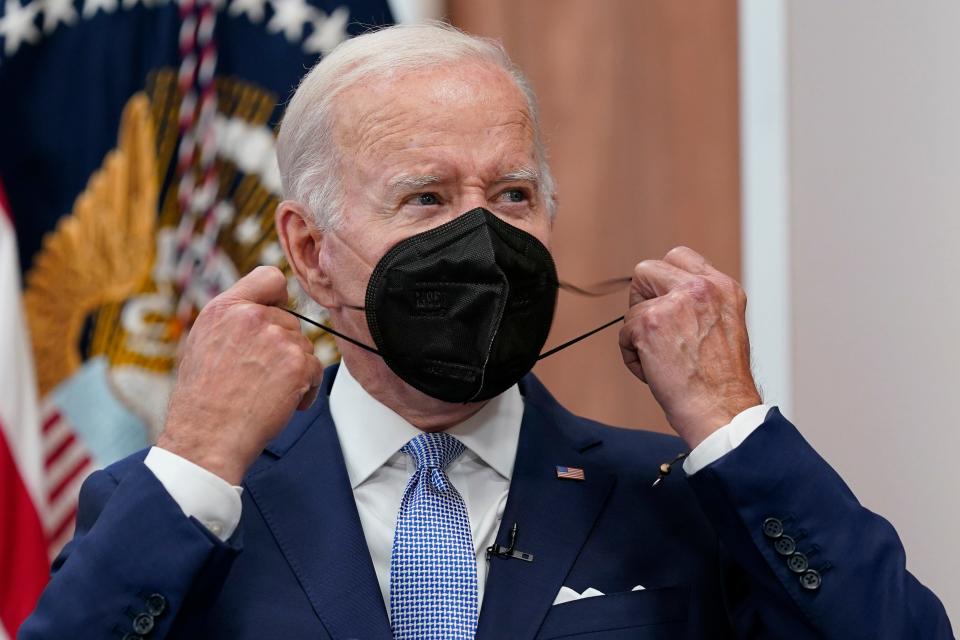
One side effect commonly attributed to Paxlovid is "rebound" — testing positive for COVID-19 or symptoms showing up again two to eight days after recovery, typically lasting about three days. Both President Joe Biden and first lady Jill Biden had rebound symptoms after taking Paxlovid for their COVID-19 infections, as did infectious disease expert Dr. Anthony Fauci.
About 14% of people test positive after testing negative and about 19% see symptoms return after a prescribed course of Paxlovid, according to one recent study that hasn't yet been peer reviewed.
The study also found this rebound in about 9% of people who didn't take the drug, suggesting it may be a feature of the body's fight against the virus that causes COVID-19, rather than a response to the medication.
In any case, the rebound is almost always mild, according to recent research, though the CDC does suggest following general recommendations for a positive COVID-19 test, which calls for isolating at home for at least five days. Typically, no further treatment is required during a rebound and it's unclear whether someone who is rebounding is contagious.
Drugs that interact with Paxlovid
Paxlovid can interact with other drugs, including common ones like blood thinners, some cancer drugs, anticonvulsants, sedatives, erectile dysfunction medications, the herbal remedy St. John's Wort, and HIV medications. (A complete list of those drugs starts on page 11 of this fact sheet.)
For people taking these medications, it is generally OK, with a doctor's consent, to pause or adjust them for five days while on Paxlovid. They can be resumed after Paxlovid's five-day treatment.
Who shouldn't take Paxlovid?
The medication should not be taken by people with severe liver or kidney disease or those who are allergic to either nirmatrelvir or ritonavir, according to the Food and Drug Administration authorization.
Does Paxlovid prevent long COVID?
The data is not conclusive on whether the medication can prevent the miserable symptoms that can linger for months or longer after a bout of COVID-19.
But one recent study of veterans, not yet peer reviewed, showed that taking Paxlovid was associated with a reduced risk of symptoms such as blood clots, heart rhythm problems, fatigue, liver and kidney disease, muscle pain, brain fog, and shortness of breath.
What causes long COVID? Researchers have some clues.
Does Paxlovid make you less contagious?
Again, there's not enough data to say that Paxlovid makes people shed less virus. But generally, people who are sicker shed more virus, so reducing the severity of illness should cut down on shedding and therefore make people less contagious.
Pfizer's data also shows that someone's viral load falls quickly once they start taking Paxlovid, Habtezion said.
Is Paxlovid FDA approved?
Paxlovid is authorized for emergency use but not fully approved by the Food and Drug Administration. Pfizer is working on the paperwork necessary for full approval.
The two drugs that make up Paxlovid have a long history and have been approved to treat HIV infections, so there's no reason to think they are unsafe.
The main hurdle for approval is showing that the drug can be manufactured consistently using safe practices, which is not expected to be a problem with a company as large and experienced as Pfizer.
Can you take Paxlovid twice?
Yes. Paxlovid can be taken with every COVID-19 infection.
Pfizer has no data on taking the medication for longer than five days to treat rebound or long COVID symptoms, Habtezion said.
Are there other treatment options for COVID-19?
Yes, there are several other treatments currently used to prevent infections from becoming severe, though none proven as effective as Paxlovid.
Unfortunately, monoclonal antibodies, which had been useful earlier in the pandemic, are no longer effective against the currently circulating variants and have been removed from the market.
Other treatments include:
Remdesivir (brand name Veklury), an antiviral that must be started within a week of the start of symptoms and is available at health care facilities as an infusion delivered for three consecutive days.
Molnupiravir (Lagevrio) is given in four capsules, twice a day for five days. It should be started as soon as possible after a positive test and no later than five days after the start of symptoms. According to one study, this oral antiviral did not reduce the risk of hospitalization and death among people who had been vaccinated against COVID-19 although it shortened the period of symptoms by about four days.
Convalescent plasma, though largely discredited for the general population, it has shown some benefit for people with COVID-19 who are immunocompromised or are receiving immunosuppressive treatment, according to the CDC.
Contact Karen Weintraub at kweintraub@usatoday.com.
Health and patient safety coverage at USA TODAY is made possible in part by a grant from the Masimo Foundation for Ethics, Innovation and Competition in Healthcare. The Masimo Foundation does not provide editorial input.
This article originally appeared on USA TODAY: Paxlovid for COVID: Side effects, drug interactions, what to know


