N.S. announces slate of changes to improve emergency departments
The Nova Scotia government has announced a long list of changes it hopes will improve care at emergency departments, including ways to ensure patients with the most urgent needs get help first, improve ambulance response times and offer more places for people to receive care.
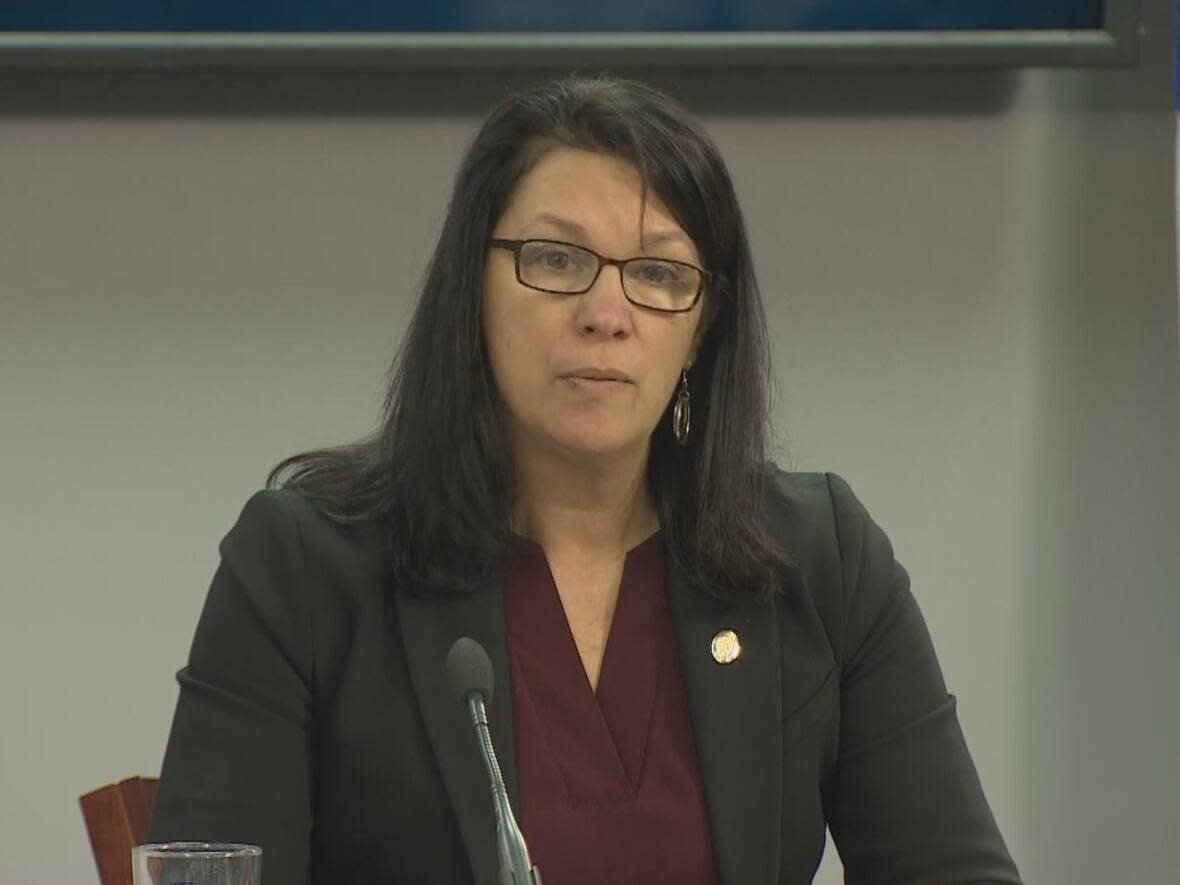
"Our health-care system has been neglected for years, for almost my entire career as a registered nurse," said Health Minister Michelle Thompson at a news conference on Wednesday. "Government after government of all political stripes has focused on efficiency and cost containment in health care, despite calls from experts and health-care workers that the system was in trouble.
"They were warned that our workforce would retire en masse, chronic disease rates were increasing, and our proportion of the population that was elderly would grow. And the lack of proper infrastructure and human resource investments would leave us in the place we find ourselves in today. But nobody listened.…
"We are investing and we are working tirelessly to reverse the tide brought on by so many years of neglect."

Karen Oldfield, the president and CEO of Nova Scotia Health, urged people with skills in health care to come forward.
"We're looking for more help. If you're a nurse or a nurse practitioner or a physician or any other health-care worker who's looking for work, rest assured, I'm looking for you. Let us know that you're available.
"Because we can do it if we all pull together with a common goal: a system that is ready, responsive and reliable."
Emergency department changes
In order to get speedier care in urgent cases, the government said that it plans to deploy teams led by doctors to triage patients and get them out of ambulances and into ERs faster.
Physician assistants and nurse practitioners will be added to teams working in emergency departments.
The province has already begun to recruit physician assistants for emergency care, and they will begin staffing the South Shore Regional Hospital and Dartmouth General Hospital immediately. Physician assistants, under the supervision of a doctor, can care for up to 62 per cent of all patients in emergency departments.
Care providers will support patients in waiting rooms by regularly reassessing their needs, and patient advocates will help patients in the waiting room by talking to them and offering food and blankets.
While volunteer patient advocates did exist in some emergency departments before the COVID-19 pandemic, they will be in place in every emergency room by this Saturday, and most of the positions will now be paid roles. Patient advocates do not need a medical background.

Virtual care will be made available to more patients with less urgent needs. Patients will be told how long their wait will be if they use virtual care, and how long it is expected to be if they wish to wait for in-person care.
Those who choose virtual care will be taken to a room where a health-care provider such as a nurse or advanced care practitioner will stay with them as they connect online with a physician or nurse practitioner.
Three hospitals have already implemented virtual care in emergency departments, and wait times for those patients have been reduced to an average of 63 minutes. Oldfield said after Virtual Emergency NS was rolled out at the Colchester East Hants Health Centre, a "goodly number" of the patients simply needed a prescription refill.
Health-care teams will also receive real-time data indicating where beds are available, and what is necessary, such as diagnostic tests, to get patients home so that beds can be freed up. That app, called a "capacity expediter," will be available in every health zone by the end of March.
Oldfield said right now, information about bed availability is tracked on paper or verbally. "Instead of waiting, waiting for someone to come down, for a phone call, for a text, whatever, that bed can be accelerated," she said.
Provincial officials were not specific about how much the changes would cost, but Jeannine Lagassé, deputy minister of the Health Department, told reporters it would be "tens of millions."
Support for paramedics
The government is pledging a tuition rebate of $11,500 for paramedics who work in the province for at least three years. Tuition costs approximately $19,500.
The training program offered by Medavie, the private company that provides ambulance services in the province, is currently offered in Halifax and Sydney, and will be expanded to Yarmouth starting in April and in Pictou in September.
A second air ambulance will be added to conduct routine transfers between Sydney and Halifax, and Yarmouth and Halifax in order to allow ground ambulances to stay in their communities more often.
WATCH | Nova Scotia announces changes to improve emergency care:
Jeff Fraser, executive director of Emergency Health Services, said he hopes to have the plane — which will be operated by PAL Airlines — up and running by mid-April. The air ambulance would have capacity for two patients, and is expected to cost $4.5 million per year.
The province said more funding will also be made available to train medical first responders, who sometimes arrive at emergency scenes first.
Offering more places for care
The province said it will provide more support for new and existing collaborative care clinics so they can see more patients. There are already 96 collaborative care clinics in the province, and 14 more will be added.
Health-care services will be expanded at pharmacies, and pharmacists will soon be allowed to order some lab services. More pharmacists will have dedicated clinic hours to assess and treat minor ailments such as joint and muscle pain, eczema, cold sores, urinary tract infections and shingles, and to renew prescriptions and provide contraception.
More hours for virtual care will be added, including on weekends and evenings, and out-of-province doctors who are licensed in Nova Scotia will be permitted to offer virtual care.
More mobile primary care clinics and mobile respiratory care clinics will be made available, as well as urgent treatment centres.
A new phone app known as a "digital front door" will be available by the end of March to help people find available health-care services that meet their needs.
Opposition parties react
Liberal Leader Zach Churchill said what's missing from the government's plan is a recruitment and retention strategy.
"They're making new positions to deal with the crisis in our ERs. Where are these people coming from?… Are we going to be robbing Peter to pay Paul to fill these positions?"
NDP Leader Claudia Chender echoed that, adding that the announcement was short on details and cost.
"We have a massive labour force issue, and there was nothing in this announcement nor in the previous infrastructure announcement that resembled anything like a staffing plan."
MORE TOP STORIES


