Public Health silent on what New Brunswickers can expect from COVID-19 this fall

British Columbia reinstated a COVID-19 mask mandate Thursday in all health-care settings and long-term care homes, while other provinces, including P.E.I., Newfoundland and Labrador and Quebec, will begin to offer updated COVID-19 vaccine boosters within the next couple of weeks.
But in New Brunswick, where 15 hospital units are closed to visitors because of COVID-19 outbreaks, 25 outbreaks have been confirmed at nursing homes and other vulnerable settings, and four new COVID deaths were reported this week, the government remains silent.
This despite the fact some New Brunswickers say their latest COVID infection was their most severe yet.
CBC News requested an interview with Dr. Jennifer Russell, chief medical officer of health, about what people can expect from COVID-19 this fall and the province's plans.
CBC also requested any modelling projections regarding COVID case counts, hospitalizations and deaths.
Continue to monitor spread
The Department of Health replied with an emailed statement.
"Public Health officials continue to monitor the spread of COVID-19 within New Brunswick through its routine reporting practices, wastewater surveillance and through genetic sequencing," Sean Hatchard said in part.
COVID-19 is a significant health risk to many New Brunswickers, he said, especially those who are immunocompromised or who fall into at-risk groups.
People should assess their own risk level and take steps necessary to reduce their risks of getting COVID, he said.
Rod Russell, a professor of immunology and virology at Memorial University in Newfoundland and vice-dean of research and graduate studies for the faculty of medicine, said he doesn't expect any major changes.
Case counts to climb, predicts virologist
"We're going to have our respiratory viruses coming back very soon, if not already, because we have kids going back to school, people coming off vacations.
"And you know, as we've learned well, as people move indoors, these bugs … get more freedom to [spread]," he said.
COVID case counts typically climb during the fall and winter, and Russell believes that will continue.
Hospitalizations, however, could be lower than previous years of the pandemic as people continue to build immunity through vaccinations and infections, he said.

Memorial University virologist Rod Russell says he doesn't believe lockdowns or mandates are necessary, but he still encourages people to get vaccinated, use rapid tests, stay home when sick if possible or wear a mask in public. (Gary Locke/CBC)
"So I think the severity of disease is just going to keep getting less and less for most people."
Although there was "a lot of hype" about the new highly mutated Omicron variant, BA.2.86, which experts initially thought might be more immune-evasive than previous variants and spread a little faster, that has since changed, said Russell.
"Basically, since the first version of Omicron, we haven't really seen anything that was … more pathogenic or made disease severity any worse."
Recent infection hit fast and hard
Cindy Colwell, 60, of Saint John, doesn't know which strain she had at the end of August, but it hit her fast and hard, she said.
She got a call one morning from a co-worker she sat beside at a meeting, advising her that she had tested positive.
By the afternoon, Colwell was feeling ill. She had a fever, was dizzy and weak, she said.
It was a full-body experience. - Cindy Colwell, Saint John resident
She also had a cough and "burning" in her bronchial tubes that got progressively worse, nausea and "intestinal issues."
"It was a full-body experience," said Colwell.
She was "kind of surprised," she said. She expected it to be more like a cold.

Cindy Colwell of Saint John says she was in bed for days with her latest COVID-19 infection, which she describes as being much worse than her first a year ago. (Submitted by Cindy Colwell)
"Where I'd had two vaccines [and a previous infection], I was thinking if I did get it, it wouldn't be as bad as the first time."
When Colwell got COVID last September, she had a fever, body aches, a sore throat and bronchial issues, but they weren't as severe as this time around, she said.
"I just, I felt so bad for at least … like four days. Really bad."
"The couple times that I did try to get up and do something, I would end up back in bed."
Her advice to anyone who gets infected is to listen to their body and rest. "Stay in bed, stay away from anyone and let yourself heal."
Antibody 'memory response' takes a few days to kick in
Russell has heard about similar experiences and admits it's puzzling because in general, the more someone is exposed to something, the less it's going to impact them, so second and third COVID infections are typically not as bad as the first for most people.
He has a theory though.
"We know that the antibody levels in the blood wane, right? This is why the vaccines don't protect us from infection as long as we'd like," only for two or three months before we're susceptible again, he said, although they do provide longer protection against severe illness and hospitalization.
"Presumably, the longer you go between [vaccines or] infections the lower your antibody levels are going to go," said Russell.
So when a new infection sets in, there's "not a lot of antibody around to contain that virus," he said.
"You might have, you know, a pretty nasty infection at the start."
By Day 3 or Day 4, however, the "memory response" kicks in, according to Russell. "Your memory T cells are ramped up, your memory B cells are ramped up and start making new antibody.
"So although the infection in the first few days might feel worse, I think it's just because there's that delay while the memory response is getting going. And then you get, I think you're getting a … quicker resolution of the sickness."
'Large pool' susceptible, potential transmitters
Many New Brunswickers like Colwell had their last COVID-19 vaccine at least a year ago.
Since July 1, the only people eligible for a shot have been those aged 65 or older and those 18 or older who are moderately to severely immunocompromised, who did not receive a spring booster and whose last shot or infection was at least five months ago, and new residents of long-term care facilities aged 18 and older who did not receive a spring booster and whose last shot and/or infection was at least five months ago.
Anybody who hasn't had a COVID booster or infection for five or six months is "definitely susceptible to getting infected again," said Russell.
"In New Brunswick you would have a large pool of people out there who are susceptible now to infection, and then they're potential transmitters as well."
Boosters encouraged to protect, reduce transmission
On Thursday, Health Canada approved Pfizer-BioNTech's updated Comirnaty vaccine, which targets the Omicron XBB.1.5 subvariant, for all Canadians who are six months of age and older.
Pfizer Canada said it expects the newly formulated vaccine to be available "in the coming weeks" before the respiratory virus season is forecast to peak.
Two weeks ago, the regulator approved Moderna's updated COVID-19 vaccine, which also targets the circulating XBB.1.5 strains, to protect those aged six months and older.
Federal officials aren't calling the shots "boosters." Instead, they view the updated options much like the annual flu shot.
New Brunswick is still finalizing its plans for fall COVID-19 vaccines, the Health Department has said.
Colwell, who got "quite sick" from her first two shots, hasn't had any boosters and doesn't plan to get any.
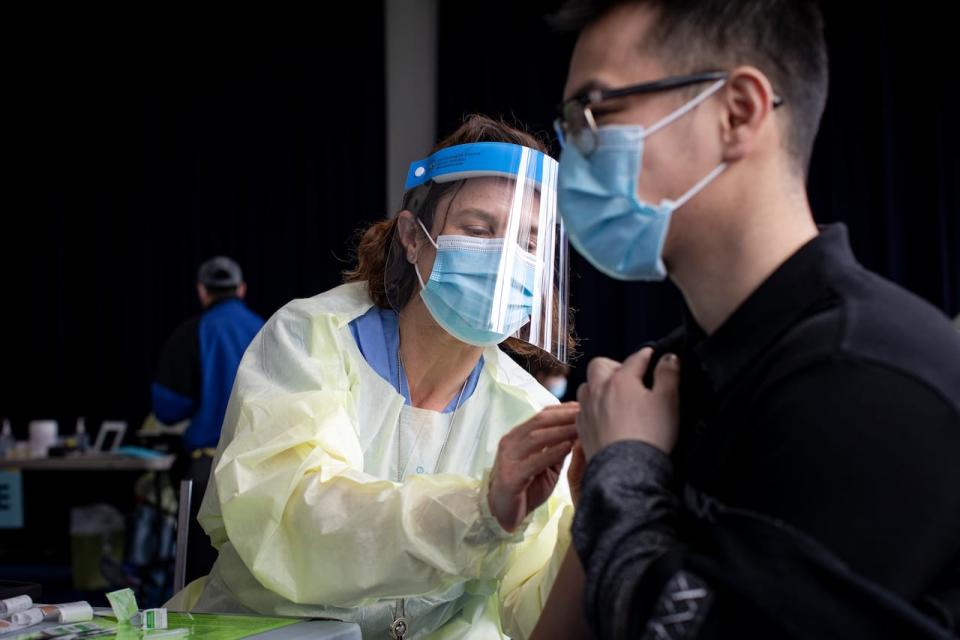
The Department of Health has said vaccination is the best tool of defence against COVID-19, as it can help reduce the risk of serious complications and hospitalizations. (Evan Mitsui/CBC)
"I just I feel like the two vaccinations were supposed to work for us. They were the be all to end all. And I still got ill … So I'm just not going to put anymore vaccines in my system."
Russell encourages everyone to get the latest booster once it's available. The closer the vaccine is matched to the current circulating strain, the more benefit, he said.
Rapid tests still effective
He also encourages New Brunswickers to continue to use rapid tests, even though the province has stopped reporting positive results.
"We should be trying not to infect others," he said. "If you have access to tests, why not use them?"
According to Health Canada, there is no evidence that new variants affect the ability of the diagnostic tests it has approved to confirm COVID-19 cases.
"A positive rapid point-of-care testing (POCT) result is a positive case of COVID-19," the Department of Health spokesperson Hatchard said.
"If you have a negative rapid POCT test result and your symptoms worsen, or new symptoms develop, you should test again in 24 hours. If it is still negative, retest in 48 hours."

New Brunswick still offers COVID-19 rapid tests for free, but Public Health says not everyone needs to be tested. (Alexandre Silberman/CBC)
Not everyone needs to be tested, he said.
"People who are ill should stay at home while sick and until their symptoms improve," Hatchard said.
Public Health recommends rapid tests for people who work in vulnerable settings or who are at risk of severe illness and may benefit from treatment such as Paxlovid.
As of Sept. 5, New Brunswick has dispensed about 8,200 of the 21,900 Paxlovid treatment courses obtained since Jan. 27, 2022.
Paxlovid is for people with mild to moderate symptoms of COVID-19 that started within the last five days and who are at higher risk of severe outcomes.
The combination of pills that can be taken at home has been shown to significantly reduce hospitalizations and deaths among people at high risk of progressing to serious illness.
'Adequate inventory'
Rapid tests continue to be available for free at various locations across the province by scheduling an appointment online or by contacting Tele-Services at 1-833-437-1424.
New Brunswick has an "adequate inventory" to meet demand "for the foreseeable future," and has not made any decisions about getting more tests, Hatchard said.
The rapid tests now being provided to New Brunswickers are due to expire "throughout 2024," he said, without providing any specifics.
Health Canada has amended the shelf life for rapid tests. "Most rapid tests can be kept and used for 24 months after their manufacturing dates."
Lung group provides rapid tests without appointments
NB Lung also has thousands of rapid tests now available at its Fredericton office, said Melanie Langille, president and CEO of the registered charity.
The tests, from the federal government's surplus, are free and can be picked up between 8:30 a.m. and 4:30 p.m., she said. No appointment is necessary.
"We'll happily send you off with two boxes of five test kits each so that you've got them on hand," said Langille. "We don't want to have any hurdles."
So far, people have been "pretty eager," she said, noting it can be difficult to determine if respiratory symptoms are COVID, a cold, the flu or RSV (respiratory syncytial virus) without rapid tests to screen.
"I think it's really important to remind people that COVID is with us … and we still need to be utilizing all these tools to protect ourselves and the community."


