$30M in mental health funding shows Sask. 'playing catch up': NDP
Saskatchewan NDP mental health and addictions critic Danielle Chartier says the provincial government's budget promises on mental health are an attempt to make up for years of inaction.
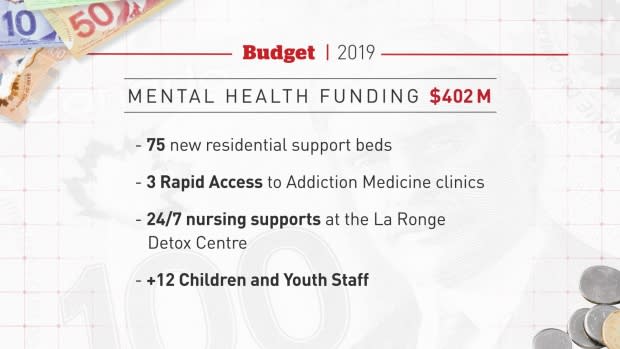
The province announced in it's annual budget Wednesday that $30 million more would go toward mental health and addictions for the 2019-20 year.
"I don't want to say too late because it is a positive measure — but it's too late for some people for sure. People have died. Make no mistake about that," Chartier said.
She said that if you don't including the $14 million for the mental health hospital in North Battleford or $6 million from the federal government, the province committed less than $10 million for new mental health initiatives in this budget.

Chartier said the province's ongoing additions and mental health crisis needs more than what the government has put forward.
"There are 22 new [inpatient addictions] treatment beds being added but we don't have any details yet on how that will better support crystal meth addiction," she said, noting the treatment of meth requires a different approach from alcohol or other drugs.
"This government has had its head buried deeply in the sand when it comes to crystal meth and opioid addiction."
Chartier said crime statistics have indicated a growing meth problem for years. Furthermore, she noted not everyone needs inpatient treatment.
"They need support in-community," she said. "They need access to addictions counselors."
Chartier also criticized the one per cent increase for community-based organizations.
"These are people who are working directly with mental health patients and they got nothing really, and they haven't gotten anything in five years," she said.
"Those organizations that provide frontline mental health care like crisis intervention services only have seen a three per cent increase in five years."
She said the province planned to cut ten per cent from its CBOs in 2017, but backtracked after public outcry.
"We're playing catch up with every other jurisdiction. Every other province is moving the bar and we are chasing after them."
Mental health patients a 'token project': activist
Advocates like Jae Blakley are also skeptical about what will actually change.
"I think putting a token bit of money into mental health at this point is just an election strategy," the mental health activist said. He's spent 12 years in and out of the mental health system.
"Mental health patients are a token project. It's easy to throw money at us and say things are getting better."
In one of numerous spending announcements yesterday, the province said its seven-bed temporary mental health assessment unit at Saskatoon's Royal University Hospital will be made permanent. It's using $1.5 million for this and renaming it the Mental Health Short Stay Unit.
Blakley criticized how it's historically operated and he worries problems will persist despite the name change.
"To keep the physical space open that's one thing, but to actually operate it correctly is a totally different matter," he said.
Blakley said the unit was supposed to help provide people in crisis quick access to treatment. However, he said his friends have waited hours in the emergency room because they couldn't get in.

"My concern is that it'll just keep operating in that way, in which case there's really no point in this funding."
Blakley said he advocates for better services because he hasn't seen improvements in more than a decade.
"There are people dying right now who don't have that voice."
Sask. launched action plan 5 years ago
Saskatchewan experts are pleased the government is starting to direct more attention to mental health and addictions, but also say it's overdue.
Dave Nelson pointed out that Saskatchewan launched its 10-year mental Mental Health and Addictions Action Plan in 2014.
"It really has not had any major investments until now," he said. Nelson is with the Saskatchewan Division of the Canadian Mental Health Association.
"What we'd really like to see is that this is the start of investments each year. Not a one time a year, and certainly not the tail end of it."

That's because there's still so much more work to be done.
Regina addictions advocate Ronni Nordal also criticized the province for being slow to implement recommendations laid out five years ago, but called the government's decision a "pleasant surprise.
"That being said the devil's always in the details."
Nordal notes many of the specifics are still unknown. She pointed out that the province is increasing beds in existing addictions treatment facilities, like Calder Centre and Pine Lodge.
It has another six new inpatient addiction treatment beds for youth slated for "southern Saskatchewan." It's still not decided where they will go.
Nordal said the budget indicates an apparent lack of "addictions treatment facilities established in new areas — which does mean people have to leave their communities" to get help.
Funding increase welcome amid addictions crisis
Saskatoon-based addictions expert Dr. Peter Butt welcomed the money because, he said, the province is not meeting the needs of its people amid an addictions crisis.
"Increasingly the use of methamphetamine has been very difficult to manage within our existing resources."
Alcohol and opioid addictions also pose great challenges he said, adding the province hasn't always relied on evidence-based treatment programs.
"I think that having these resources creates a responsibility to use them in a wise and efficient way," he said. "We need to be much more assertive in how we deliver care."
He wants to see the system improved — rather than just an increased capacity.
Butt is critical of current care models, which typically involve a seven-to-10-day detox that might be followed by a 21-to-28-day rehab program.
"It's a bit of a drop in the bucket."
Butt said it can take years to recover from substance use disorder.
He said it's positive money is going toward 50 beds for patients transitioning out of detox. He's hopeful additional resources will go toward supporting people in their transitions between different phases of recovery.
Butt said support must extend far beyond treatment beds and into the psychosocial realm of care to truly tackle the root of addictions and stop the crisis.

