Sask. medical students to ask provincial government to pay for and distribute naloxone
University of Saskatchewan medical students want the provincial government to pay for and distribute naloxone nasal spray kits amid an unprecedented level of drug overdose deaths in the province.
Students for Harm Reduction and Informed Policy (SHRIP), along with representatives from Regina's Nēwo-Yōtina friendship centre, met with the Opposition NDP Monday to share their plans to help reduce drug overdose deaths in the province.
In 2022, 421 Saskatchewan residents died from drug overdoses, the highest on record.
In January 2023 alone, there were 55 suspected drug overdose deaths in Saskatchewan, according to the provincial coroner's office, up six from January 2022.
"This is probably one of the most prevalent public health crisis we've had in Saskatchewan in recent years other than COVID-19," said Ryan Krochak, SHRIP Regina president.
Krochak said that in addition to the naloxone nasal spray kits, the province must fund safe consumption sites.
"We need to ensure we have harm reduction and that we're keeping people alive until they are ready to access treatment," Krochak said.
He noted that mental health concerns, drug decriminalization and poverty reduction are critical to addressing drug problems.
"It's a complex problem and it doesn't have a simple solution."
He also added that he understands the limitations of naloxone, but said it's an important tool, especially at this time.
SHRIP is scheduled to meet with Health and Addictions Minister Everett Hindley on April 4. It has the support of key health organizations including the Saskatchewan Medical Association, Saskatchewan Union of Nurses, AIDS Program South Saskatchewan and the Regina branch of the Canadian Mental Health Association, Krochak said.
"We need them to realize that there's a drug problem going on. It's been going on for a long time and it's not being addressed," said Emile Gariepy, harm reduction manager and primary care paramedic at Nēwo-Yōtina.
The centre provides a safe injection site, new needles and test strips for drug users.
"We're getting completely overloaded here," Gariepy said, explaining that as many as 400 people use the centre monthly as a safe injection site.
He supported SHRIP's push for free nasal naloxone, saying it is much easier for non-medical staff to administer during a drug overdose.
"Unfortunately some parents and children will be involved with drug abuse, and how is a child supposed to know how to use a needle to open up an ampule?"
In briefing notes to Hindley, SHRIP said the government should not only fund naloxone nasal spray, but actively distribute the drug instead of "passively" requiring people to pay for and pick up kits at pharmacies.
"At a time when Saskatchewan's health infrastructure is overwhelmed, [naloxone's] no assembly and intuitive nature can ensure that nearly all community members are able to rapidly intervene during an overdose and prevent any serious medical complications requiring lengthy ICU admissions from lack of oxygen to the brain," SHRIP's briefing notes to Hindley stated.
During Monday's question period, Hindley said the province is working on a pilot project drug task force to help deal with the opioid crisis.
"And [we] are starting to fund, through a pilot basis here, overdose outreach teams to try to reach people where they're at, in their communities, meeting them where they need those supports," Hindley said.
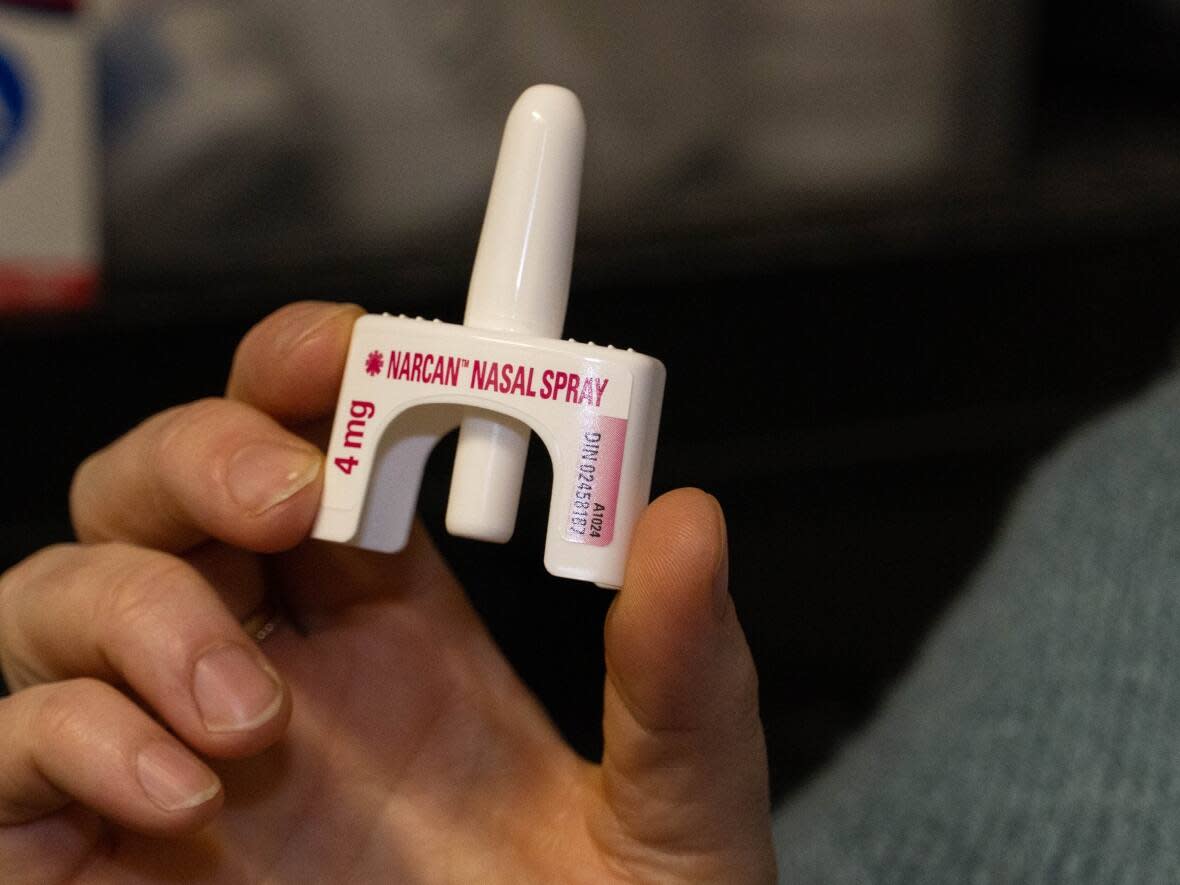
According to SHRIP, the Health Canada-approved nasal spray has several advantages over injectable naloxone kits.
SHRIP says spray acts quicker, lasts longer and has a higher peak concentration compared with injectable naloxone. It also eliminates the need to dispose of potentially contaminated needles.
Naloxone spray is more expensive than an injectable version, but said it saves money in medical complications, like ER visits and intubation, SHRIP says.
SHRIP is receiving support from medical and addiction groups, which agreed that naloxone nasal spray could reduce the number of drug overdose deaths.
"This is a laudable effort and one that is very close to the SMA and physicians of the province," Saskatchewan Medical Association president Dr. John Gjevre wrote in a news release.


