Type 2 diabetes crisis can be controlled. These solutions are how we get there.
Editor's note: Part five of a five-part USA TODAY series revealing why America hasn't solved its long struggle with Type 2 diabetes.
The free food box that arrived on Barbara White’s porch every two weeks for a year was a godsend.
It was always a happy surprise when she pulled back the tape and wrenched open the cardboard. She never knew exactly what meal fixings she might find inside: meat, olive oil, seasoning, vegetables. Her favorite was the spinach salad with strawberries.
Eating better helped her feel better. She had more clarity. Fewer aches and pains. No more waking up with a headache. Her A1C, a measure of her Type 2 diabetes, improved, allowing her to cut back on medications with unpleasant side effects.

“It’s been a life changer for me,” said White, 64, a former beautician and retired special education classroom assistant from Stockton, California.
Such food boxes, in her case sponsored by the Abbott Fund, may be the beginning of a solution to America’s diabetes dilemma.
But as with all the other potential solutions, the main challenge remains getting such programs to people who need them.
Diabetes has to be fought on many fronts at once, experts said, from a food system that provides far too many unhealthy calories to a medical system that offers limited and unequal care to the need for individuals to be empowered and motivated to help themselves.
More in series: American can prevent (and control) Type 2 diabetes. So why aren’t we doing it?
Preventing diabetes is an obvious first step.
At Intermountain Healthcare, an innovative nonprofit system based in Salt Lake City, scientifically validated prevention programs have reached thousands of people at risk for diabetes, helping them improve their nutrition, increase physical activity, prioritize sleep and learn they have the power to avoid a diabetes diagnosis.
The programs save the health care system $3,500 per person in the first year alone.
Still, even within Intermountain, only 1 out of 5 eligible patients gets referred.
“Despite all the success we’ve had,” said Dr. Liz Joy, formerly Intermountain’s senior medical director for wellness and nutrition, “we have a ways to go.”
The Diabetes Dilemma
Type 2 diabetes rates continue to climb, despite well-known treatments and prevention approaches. To better understand why, USA TODAY's health team traveled across the country, talking to researchers, clinicians and patients. They found people with diabetes often must fend for themselves against systemic barriers and a difficult disease.
So does everyone else.
Roughly 1 in 3 Americans – 96 million adults – have prediabetes but just 2% to 3% are offered the kind of help shown to prevent progression to full-blown disease.
Similarly, offering healthy food to people like White could counteract many of the worst effects of diabetes and save money overall. Poor diet, including too much meat and refined grains, has been shown to drive Type 2 diabetes. Providing nutritious meals to those with health problems and movement limitations could save more than $13 billion in the first year alone.
The same story, as we’ll see, can be told for a whole health and education program in Hardin, Montana on the edge of the Crow Indian Reservation. And new-generation medicines and medical devices also offer tremendous hope – if only the people who need them can get access.

“We know how to reduce the penalties of diabetes, but it takes money and resources to do so,” said Dr. David Nathan, who directs the Diabetes Center at Massachusetts General Hospital in Boston and has been an adviser to the federal program almost since its inception. “I think the answer really is a cultural and societal one.”
What keeps him going, Nathan said, is the knowledge that by helping people keep their blood sugar levels close to the normal range, he can reduce their risk of developing “horrendous” long-term complications like vision loss, kidney failure, amputations and heart disease.
“We can take the teeth out of diabetes and make it a safer disease,” he said. But “it takes a lot of drugs and a lot of attention and puts a big burden on the patients.”
'At the crisis level'
Adequately addressing diabetes, particularly preventing it, would save American taxpayers immense sums.
In his 2021 doctoral dissertation, Bryan Tysinger, who now directs Health Policy Simulation at the University of Southern California’s Schaeffer Center for Health Policy and Economics, found that eliminating all new cases of diabetes until 2050 would save Medicare and other government programs $2.6 trillion.
And that’s just the financial cost, not to mention the personal burden of feeling sick, worrying about blood sugar levels and the dangerous downward spiral.
More in series: Diabetes runs deep in rural Mississippi. Locals have taken to growing their own solutions.
Diabetes intersects so many other problems in America – income inequality, racial and class bias, lack of access to nutritious food, housing instability and a medical system that leaves many patients feeling uncared for and unwell. Solving the problem of diabetes would go a long way toward solving many of these problems as well, said Dr. Bisola Ojikutu, executive director of the Boston Public Health Commission.
Addressing diabetes, “is for the betterment of our entire country, for the benefit of individuals, even if you’re not necessarily at risk (for diabetes yourself),” she said.
Type 2 diabetes, like many other health problems, disproportionately affects people with lower incomes and darker skin colors. But such disparities cost everyone, regardless of their position in life, Ojikutu said.
A June report found inequities cost the state of Massachusetts alone $5.9 billion per year in lost productivity and the expense of treating chronic diseases.
“It is an enormous amount of money that is being wasted over these kinds of issues,” she said. “It’s easy to ignore the fact that (diabetes) is at the crisis level, but at some point, we have to say, we can’t ignore it anymore.”
A medicine revolution
The newest generation of diabetes medications has the potential to transform care for millions, several experts said.
Drugs like Ozempic and Mounjaro have gotten more public attention for their ability to help people lose unprecedented amounts of weight, but this class of drugs, known as GLP-1 receptor agonists, are also very effective diabetes drugs.
They can lower A1C levels by 1% to 1.5% or more within just three months, which brings many people with diabetes to a level considered well controlled, said Dr. Joshua Joseph, a diabetes expert at the Ohio State University College of Medicine and chair of the clinical affairs core committee of the Endocrine Society, a professional organization.
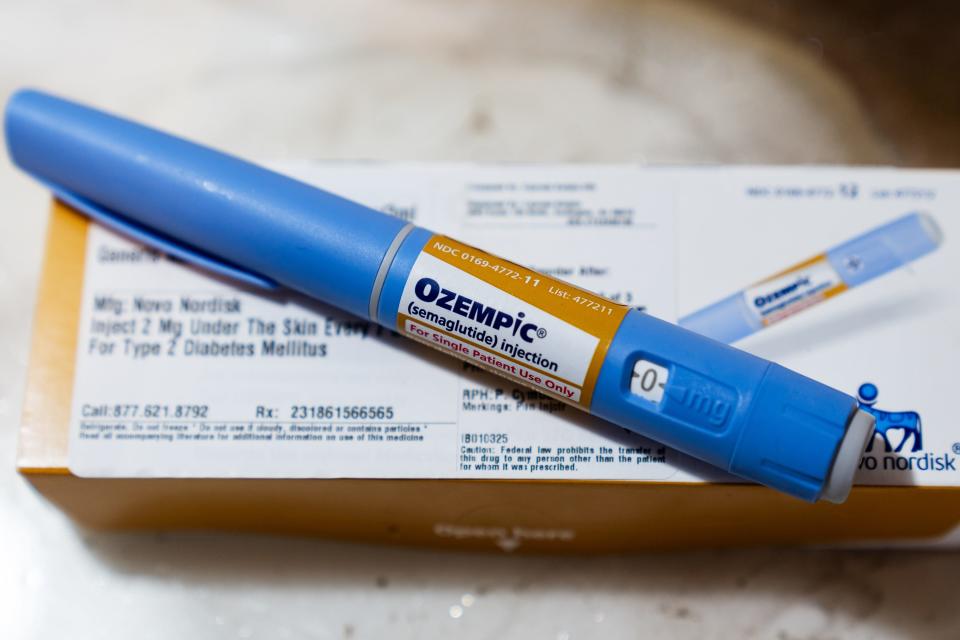
Because they work differently than other diabetes drugs, they can also be used in combination, compounding the benefit of other medications, like insulin and metformin.
The GLP-1 drugs have also been shown to reduce cardiovascular events like heart attacks and strokes, which are major killers of people with diabetes. And they can help people lose 15% or more of body weight, which, long-term, may also help prevent other health problems, including some cancers.
More in series: A diabetes disparity: Why Colorado's healthy lifestyle brand isn't shared by all
Still, not everyone who needs a GLP-1 drug for diabetes can get one. Only about 20% of eligible people with diabetes have access to them, said Dr. Robert Gabbay, chief scientific and medical officer for the American Diabetes Association.
And that doesn’t count anyone with obesity who might be able to avoid diabetes if they could get help losing some excess weight.
Covering weight-loss drugs for those at risk for diabetes would save Medicare $175 billion over a decade, largely by reducing hospital inpatient care demands and the demand for skilled nursing care, according to an April study from Tysinger and his colleagues at the University of Southern California. If private insurers also covered weight-loss medications, the savings would jump to $245 billion, they found.
But insurance companies often balk at the GLP-1’s $900-or-more-per-month price tag, even for people with diabetes, and coverage is much more limited for those who have obesity but not diabetes.
Joseph said he recently had to fight to keep coverage for a diabetes patient who described her GLP-1 medication as transformative. “She feels like she’s gotten her life back,” Joseph said.
In his medical practice, one person devotes nearly all of their time to requesting prior authorizations so patients can access these diabetes medications, Joseph said.
“I do think in many ways this medication will help us manage the toll of diabetes in the United States,” he said.
'Life-changing' glucose monitoring
Continuous glucose monitors also can make a profound difference for many patients with Type 2 diabetes.
Experts say many more could benefit if given the opportunity.
Dr. Sean Oser, a primary care physician in Colorado, chuckles as he recounts the story of one patient whom he’d told for years that eating foods like pizza would spike his blood glucose. Then, he gave the man a continuous glucose monitor.
At his next visit the man told Oser: “You wouldn’t believe what happens when I eat pizza!”

“The conversations we had were not the best way for him to learn that information,” Oser said. “Seeing it in real-time was life-changing for him.”
The educational aspect of the monitors is also what impresses Dr. Melanie Jackson, an endocrinologist at Samaritan Health Services in Corvallis, Oregon.
For many of her patients, “I put them on a sensor and they come back and they’ve dropped their A1C often a full percentage point just because they can see that their blood sugar is high,” she said. “They do so much better with their own management when they can see the data.”
A continuous glucose monitor can help the patient and doctor see how much time the person spends “in range” – with blood sugar that’s not too high and not too low, said Oser, associate director of the primary care diabetes lab at the University of Colorado School of Medicine in Aurora, near Denver.
More time in range means patients are less likely to risk short-term health problems, such as dizziness, confusion and life-threatening seizures, as well as long-term consequences like kidney disease and blindness.
With a monitor, a doctor can ask a patient what they were up to on Saturday when their glucose levels were all over the place, or get an early warning sign when their blood sugar is trending dangerously high or low, Jackson said.
In one case study in the U.K., monitor use among 20 patients followed for a year reduced hospitalizations from 15 to zero, primary care visits by half, outpatient appointments by 66% and saved as much as $1,300 per person, according to data from Dexcom, one of two manufacturers of continuous glucose monitors.
That should be enough to convince public and private insurers to cover the cost of continuous glucose monitors, but so far, their availability has been very limited.
Many patients don’t know they’re eligible and many primary care physicians, who manage 90% of Type 2 patients, don’t yet recognize the benefits of continuous glucose monitors, Oser said.
Oser and his wife are leading a three-year study introducing continuous glucose monitors into 60 primary care clinics and community health centers in Colorado.
“I think there’s a thirst for using this new technology and being able to enhance patient care with the best available tools,” said Oser, who was amazed by the number of clinics that quickly volunteered to join the study.
More in series: The steep cost of Type 2: When diabetes dragged her down, she chose to fight
He hopes that educating primary care practices will help provide more equitable care. Studies show patients who are Black or Hispanic are less likely to have access to continuous glucose monitors than those who are white or Asian, but people with disadvantaged backgrounds because of race or economics do just as well as anyone else when given access to the technology, he said.
For Jackson, continuous glucose monitors along with the GLP-1 drugs can relieve some of the burden of diabetes.
“The combination of a sensor, a patient’s willingness to really engage and a strong medication can make a huge difference,” she said.
Education in action
Chronic disease management nurse James Brown adds education to the mix.
In Hardin, Montana, Brown educates his patients – mostly ranchers, farmers, miners and welders – on how to self-manage their diabetes.
It’s tough to eat healthy in rural western towns like this one, where the only restaurants are fast-food chains with lines out the door at mealtimes. Hardin's sole grocery store stocks mainly processed foods and snacks. The One Health-Bighorn clinic where he works offers vouchers for the local farmer’s market, but it only operates one month a year.
Still, Brown said, he can make good progress with patients, by offering a two-hour education program along with a continuous glucose monitor and prescriptions.
“You can see the relief on people’s faces when you explain (diabetes) … is not a death sentence," he said. "They can have control over the outcome."
One Health, a consortium of community health centers in central Montana and northern Wyoming, originally focused just on treating diabetes but then “zoomed out a little bit and created a really neat curriculum for wellness and how to think about health broadly," said Dr. David Mark, the organization’s CEO.
The program is designed around the needs of the local, largely Native American community in a very rural region. Patient resource specialists connect people to community services of all types, not just those related directly to health.
Taking this “zoomed out” approach to chronic health problems is more effective and saves money in the long run, Mark said. Of 58 One Health patients whose A1C values stabilized or improved, outpatient expenses didn't increase significantly despite more regular monitoring, and their inpatient admissions declined, providing potential savings of about $5,500 a year.
“We pay for it up front or we pay for it at the back end, and it’s much more cost effective to pay up front,” Mark said.
Other diabetes education programs report similarly effective results.
At Piedmont, which serves 80% of Georgia’s population, about 5,000 patients have received a three-session diabetes education program provided by Epic.
About 80% of those who complete the classes see a substantial drop in their A1C. More than 15% drop a full percentage point, said Dr. Jim Latimer, Piedmont’s chief medical informatics officer for ambulatory services.
“I’m thrilled that the program we’ve developed has been shown to be able to have an effect,” he said “We want to expand it further so that we can help more.”
Back in Montana, Brown said his biggest challenge is getting people with prediabetes or diabetes to start making lifestyle changes. “Breaking through the veil of denial,” as he put it.
Brown, who exercises regularly and takes metformin and Ozempic for his own diabetes, said he encourages his patients to look out a decade. “Do you see yourself on dialysis or taking your grandkids fishing and hunting?” he said. “If you go to dialysis three times a week and you’re wiped out, you don’t even enjoy playing with your grandchildren.”

Praise for the change
Back in California, White said the most important things she’s learned from her year of food boxes, nutrition classes and an ongoing virtual support group was how to enjoy food again – both for herself and to share with others.
She talks with pride about the special “sock-it-to-you” fish soup that was her late-nephew’s favorite. She used to load it up with cheese, salt and noodles. Her nutrition classes taught her that wasn’t the healthiest. So now, White loads it with cabbage and other vegetables instead. It’s just as delicious, but cheaper, lower in calories and “it’s not going to give you high blood pressure,” she said.
Once this spring, the youngest of her four grandchildren, 5-year-old Ethan, noticed she forgot to include the broccoli in her soup. “He gave me this cartoon look with his hands up and said, “I Like Broccoli!” she said. “Believe me, next time I made sure I put that broccoli in. I was so happy that he knows what he likes and he knows that it was missing.”
White was inspired by the generosity of the biweekly food boxes, valued at $40 each and provided through a collaboration between the Abbott Fund, the philanthropic foundation of the global health care company, Stockton Emergency Food Bank and the Community Medical Centers. Though far from wealthy, White spends whatever extra she has buying nutritious food for neighborhood seniors.
"It's my joy to make them happy,” she said.
Even her community can tell she’s eating healthier, White said. At the grocery store, the checkout clerk comments about her being a “healthy eater” and a fellow customer once told her “you got all the healthy stuff.”
When other people notice, White said, “that’s when you know you’re changing. It’s a blessing. Truly a blessing.”
Contact Karen Weintraub at kweintraub@usatoday.com.
This story is part of a reporting fellowship sponsored by the Association of Health Care Journalists and supported by the Commonwealth Fund.
Health and patient safety coverage at USA TODAY is made possible in part by a grant from the Masimo Foundation for Ethics, Innovation and Competition in Healthcare. The Masimo Foundation does not provide editorial input.
This article originally appeared on USA TODAY: Type 2 diabetes can be prevented. Why are millions left without help?


