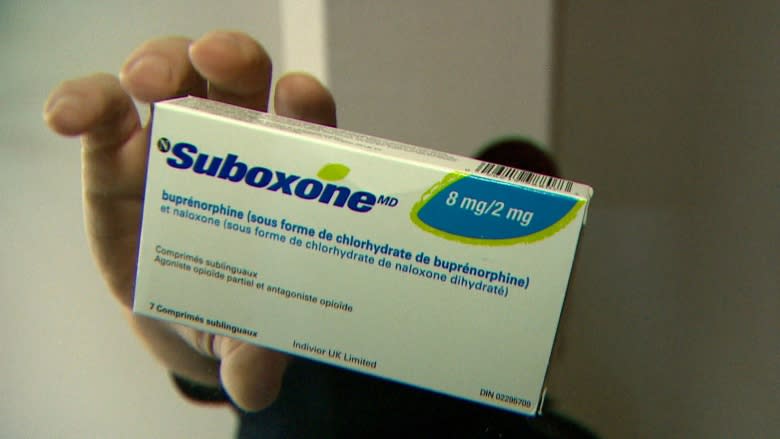
Suboxone recognized as new first line of treatment for opioid substitution therapy
Jurisdictions in the United States are now using Suboxone as an alternative to methadone to fight the opioid crisis, and Canadian experts are pushing health-care providers to do the same.
Suboxone, like methadone, is a form of opioid replacement therapy and with 161 people dying of illicit drug overdoses in March of this year, front-line workers in B.C. see the treatment as a potential solution.
"It's not a new medication but it's newer in comparison to methadone and it's just starting to become recognized among, not just addictions physicians, but all health-care providers," said Dr. Seonaid Nolan, the medical director of the addictions program at St. Paul's Hospital and a clinical researcher with the B.C. Centre on Substance Use.
But the complex nature of Suboxone and the shortage of those trained to administer it are just some of the barriers to the drug being more widely distributed than it is in B.C, according to Nolan.
Dr. Mark McLean, the medical lead of the Rapid Access Addictions Clinic at St. Paul's, said the complexity of the drug is one reason why some doctors are hesitant to prescribe it: It can only be taken during a specific stage of withdrawal. Otherwise, it can cause severe sudden withdrawal.
Increased education for providers
The B.C. Centre on Substance Use launched a free online addictions training program for frontline care providers to update their knowledge on evidence-based care.
The program includes education on the prescribing of Suboxone, and Nolan said she's seen an increase in primary and emergency care providers prescribing the treatment.
In San Francisco, Mayor Mark Farrell has announced a $6 million investment in a Suboxone outreach team of 10 people who will go out into the community to prescribe and administer the drug.
Nolan said this innovative form of treatment makes a lot of sense, in terms of bringing treatment to individuals rather than expecting them to consistently show up for treatment, because the lives of this patient population don't necessarily allow for that kind of regulation.
National guidelines on Suboxone
In New York City, Dr. Chinazo Cunningham has been prescribing Suboxone for years as an alternative to their restrictive, highly regulated methadone treatment options.
"There's very little possibility to expand methadone treatment, however the Suboxone … is one way that any provider in any setting in the United States can actually provide treatment," Cunningham told The Early Edition's Stephen Quinn.
The B.C. Ministry of Health relaxed restrictions on Suboxone in 2016 and a report from the B.C. Centre for Substance Use recommended the drug as the preferred first line of treatment for opioid use disorder.
It's now been adopted as a national guideline, according to Judy Darcy, B.C.'s minister of mental health and addictions.
"Methadone is still used, but Suboxone has been found to be just as effective and, in fact, safer and works more quickly for patients who are suffering from opioid addiction," Darcy said.
"As we have more people trained in more communities across B.C. that we'll see increased use of Suboxone as well as … the other alternatives and injectable opioid substitution therapy."
She has seen an 80 per cent increase in providers who prescribe Suboxone and a new regulation now allows nurse practitioners to prescribe the treatment as well.
"We're really being very aggressive in increasing the number of providers, because we need to find alternatives to the street drugs that are killing people at a rate, often, of four people a day."
To hear the full interviews listen to media below:
With files from The Early Edition